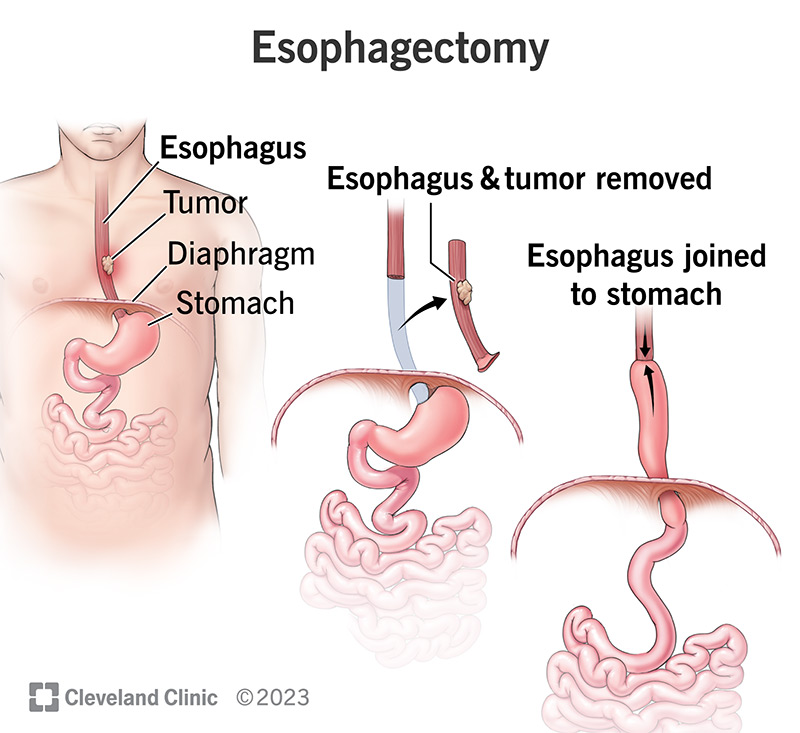
An esophagectomy is a surgery to remove all or part of your esophagus (the tube through which food travels from your throat to your stomach). Surgeons usually perform this procedure to treat esophageal cancer. It’s an extensive surgery that involves removing the damaged tissue and reconstructing your digestive system without it so you can eat.
An esophagectomy is surgery to remove all or part of your esophagus. This is the tube that carries food and liquid from your throat to your stomach. You may need this surgery if you have esophageal cancer or your esophagus isn’t working as it should to help you swallow.
During the procedure, your surgeon will remove the damaged part of your esophagus and some of your lymph nodes (if you have cancer) for testing. Then, they’ll stitch together the remaining tissue to reconstruct your digestive system so you can eat.
All esophagectomies remove your esophagus. But, your surgeon’s specific technique depends on many factors, including where the tumor (or damage) is located and the specific procedure that benefits you most.
Your surgeon may perform traditional open surgery, which involves making a single incision (cut) into your skin or tissue to access your esophagus.
They may perform all or part of your surgery using a minimally invasive technique called laparoscopic surgery to access organs in your abdomen. Laparoscopy involves accessing your esophagus and operating through a few 1-inch incisions. Your surgeon might also use thoracoscopic surgery, a similar minimally invasive procedure to access organs in your chest.
Common techniques include:
Ask your surgeon to explain their approach and why it’s the best option for you. They’ll help you understand how the procedure will impact your experience and recovery time.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
An esophagectomy is the most common surgery to treat esophageal cancer. It also treats conditions that increase your risk of cancer, like Barrett’s esophagus, and benign (noncancerous) conditions that prevent your esophagus from working as it should.
An esophagectomy is a major surgery with a long recovery time. Before having this procedure, you may need many tests to ensure you’re a strong candidate for surgery. You may need to change some parts of your daily routine to increase the likelihood of a successful surgery.
You may need to:
In the days leading up to your procedure, follow your provider’s guidance on:
Advertisement
Before surgery, you’ll get anesthesia to put you to sleep so you don’t feel any pain. Your surgeon may place an epidural catheter into your back to help with pain management after surgery.
Regardless of the type of esophagectomy, you’ll need a feeding tube to provide nutrition as you recover your ability to swallow. Your surgeon will insert the tube into your stomach or small intestine.
You’ll also have a nasogastric tube, a drain that goes in through your nose. This tube suctions out excess air in your stomach, which helps you heal. You may need chest drains to empty fluid that collects in your chest cavity, as well. This also helps you heal.
An esophagectomy is a complex surgery. Most surgeries take around three to six hours.
After an esophagectomy, your care team will move you to the intensive care unit (ICU) for a day or two. You’ll start receiving nutrition through the feeding tube, and your care team will adjust the epidural to manage pain. You may be in the hospital for up to two weeks after surgery.
While in the hospital, you’ll transition to taking liquid pain medications through the feeding tube. Your care team will remove your nasogastric tube and drains once you don’t need them. To help you heal:
In this care phase, you’ll see many healthcare providers, including your surgical team, respiratory therapists, physical therapists and social workers. They’ll help prepare you to go home.
Advertisement
It’s common to experience side effects after surgery. Your care team will monitor your health and help manage your symptoms. Side effects include:
These symptoms typically improve as you heal, but some (like indigestion problems) may remain.
The main risks of an esophagectomy include:
Alert your provider if you notice any signs of a complication.
Life after an esophagectomy takes lots of adjustment. Depending on your condition and the type of surgery you had, you may need visits from a care nurse to guide you through the recovery process at home.
You’ll likely continue eating and drinking through a feeding tube for up to two months. Eventually, you’ll transition to a liquid diet and then soft foods. Once you’ve healed and your care team says it’s safe, you can transition to a meal plan with most of the foods you ate before surgery.
You may need to change how often you eat and your portions. You’ll need to account for a shorter digestive system that’ll need more time to digest what you eat. For example, you may need to eat several small meals a day instead of three big ones. You may need to cut your food up into small pieces and chew slowly. Taking care can prevent indigestion symptoms, like heartburn.
Be patient with yourself as your body adjusts to these changes.
You may need to stick to only taking sponge baths first. Your healthcare provider will let you know when it’s safe to transition to showers or baths.
Part of cleaning yourself will involve cleaning around your feeding tube and flushing it. Your care team at the hospital or a home health nurse will teach you how to do this.
You’ll also need to learn how to clean and dress your wound and check for signs of infection. Contact your provider if you notice:
You likely won’t feel like exercising during recovery, but it’s important to get moving to prevent blood clots. At first, your healthcare provider may recommend taking brief walks every few hours just to stay in motion.
It’s essential to follow your provider’s instructions about which activities are safe and which aren’t. For example, even lifting something light (10 lbs.) can be too much when you’re recovering. Movement is good for recovery, but overexertion isn’t.
It may take a year or two to feel like you’ve healed and adjusted to life post-surgery. Still, everyone’s situation is different. Your condition before surgery greatly impacts your recovery time.
Instead of thinking of recovery as one time period, it can be helpful to think in terms of milestones, including the day when you’re eating the foods you enjoy and the day when you don’t have exercise restrictions. Every milestone matters.
Call your provider if you have any questions about caring for yourself, your incisions or your feeding tube. Contact your care team if you:
Go to the emergency room (ER) or call 911 immediately if you:
A note from Cleveland Clinic
Having any organ removed is a life-changing experience. Learning that you’ll need to have your esophagus removed may make you afraid, or it may overwhelm you with questions: Will it cure my cancer? Will it allow me to live longer? Will I be able to eat like I want to? How much time will I need to recover and adjust?
Keep in mind that an esophagectomy isn’t a one-size-fits-all surgery. Your recovery depends on your general health before the procedure and your unique diagnosis. Ask your surgeon how to plan for this procedure in the short and long run so you’re prepared for every milestone as you heal.
Last reviewed on 10/26/2023.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy