Portal vein thrombosis (PVT) is the formation of a blood clot in the veins of your liver. People with cirrhosis have a higher risk. You may not realize you have PVT until complications like portal hypertension develop. You may then have symptoms like vomiting blood and rectal bleeding. Healthcare providers treat PVT with medications and procedures.
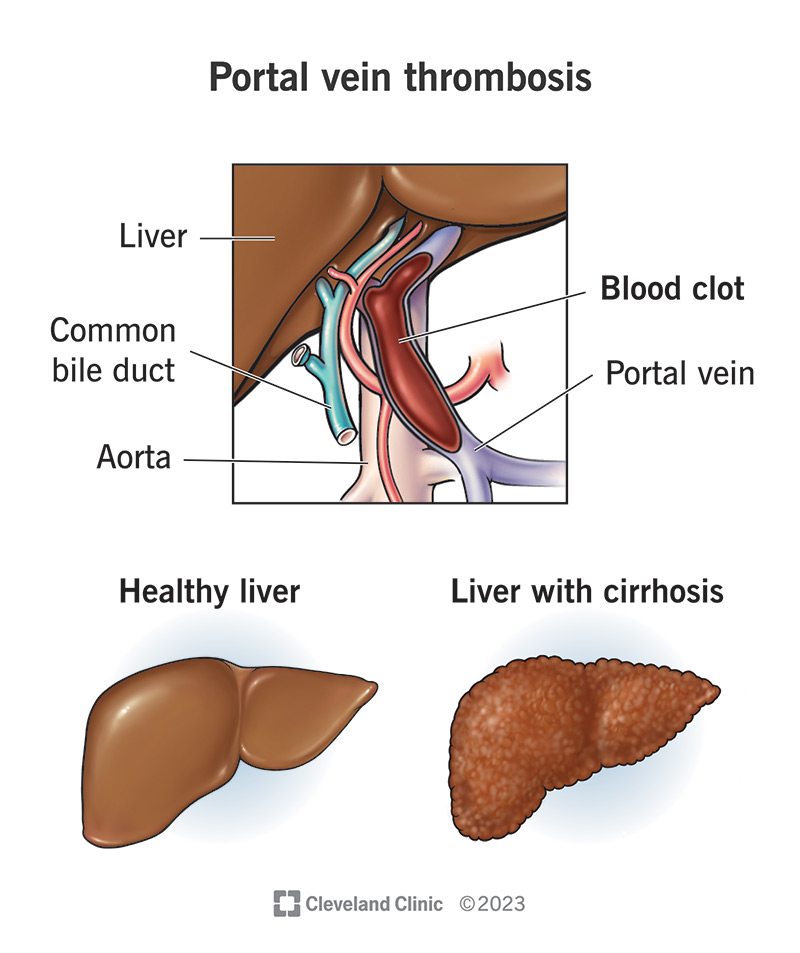
Portal vein thrombosis (PVT) is the formation of a blood clot (thrombus) that narrows or blocks your portal vein. This vein carries blood to your liver from organs in your abdomen (belly). Clots can also develop in your portal vein’s branches (inside your liver) or the blood vessels that drain into your portal vein (superior mesenteric vein and splenic vein).
Portal vein thrombosis is a serious condition, but it often causes no symptoms. So, you may not know you have a blood clot until a healthcare provider finds it through testing or you develop complications, like portal hypertension. Such complications are serious and life-threatening without treatment. Common symptoms include vomiting blood and rectal bleeding (blood in your poop). If you have these symptoms, seek medical care immediately.
People with cirrhosis face a higher risk of portal vein thrombosis and its complications. Many other medical conditions, like certain blood clotting disorders, can also raise your risk. It’s important to talk to a healthcare provider if you have risk factors for portal vein thrombosis. Your provider will make sure you receive appropriate screenings to diagnose and treat issues as early as possible.
Healthcare providers classify PVT into two main types based on who’s affected:
This distinction is important in managing the condition. For example, providers often make treatment decisions based on whether or not you have cirrhosis.
Cirrhosis can also affect your prognosis (outlook) by raising your risk for complications. However, providers continue to learn more about both types of portal vein thrombosis and how to lower your risk for complications. Talk to your provider about your treatment options and what you can expect.
Portal venous thrombosis is relatively uncommon in people without liver disease. But the risk is higher among certain groups, including people with cirrhosis. As many as 1 in 4 people with cirrhosis develop PVT. This is because scar tissue in your liver slows down your blood flow, and slow blood flow raises your risk of a blood clot.
Complications depend on the exact location of the clot and any underlying conditions you have. Possible complications include:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Many people have no symptoms. Healthcare providers often diagnose this condition through imaging tests ordered for other purposes.
However, you may have symptoms if complications develop. Symptoms can include:
Healthcare providers call this condition “multifactorial.” That means two or more factors usually interact to cause it.
A blood clot may form in your portal vein due to:
Many different medical conditions can make your blood more likely to clot and/or slow down blood flow through your liver. These include:
In addition, certain abdominal surgeries (like splenectomy) can raise your risk by injuring the lining of your vein.
Advertisement
Healthcare providers diagnose this condition through a comprehensive physical exam and testing. They’ll also ask about your medical history to learn if you have risk factors for portal vein thrombosis.
Your provider may order tests to diagnose portal vein thrombosis and check for complications. Possible tests you may need include:
The results of these tests will guide your treatment plan.
Healthcare providers decide treatment on an individual basis. They tailor treatment to your needs based on many factors, including:
Treatment options include:
Talk to your provider about the benefits and risks of treatment in your individual situation.
Advertisement
You can’t always prevent blood clots, including those in your portal vein. But here are some actions you can take to lower your risk:
Your healthcare provider is the best person to ask about your prognosis. They’ll tell you what you can expect based on your individual situation. The survival rate and life expectancy for portal vein thrombosis can vary based on:
In general, prompt diagnosis and treatment can help improve your outcome.
See your provider for yearly checkups. Contact them sooner if you have any new or unexplained symptoms.
If you have one or more risk factors for portal vein thrombosis, it’s a good idea to discuss these with your provider. Ask about your individual level of risk and what you can do to lower it.
Acute gastrointestinal (GI) bleeding can be a complication of portal vein thrombosis. Symptoms are often sudden and severe. Call 911 or your local emergency number if you have:
Some questions that may help you learn more about your condition include:
Learning you have a blood clot can be frightening. In the case of portal vein thrombosis, you might wonder which complications could occur and how serious they could be. Write down your questions and share them with your healthcare provider. Get all the information you need to learn about your condition and treatment options. Together with your provider, you’ll navigate the path toward recovery.
Last reviewed on 03/14/2024.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy