If you have meibomian gland dysfunction, the glands near your lids aren’t producing enough oil or good quality oil. The oil is one of the ways that your eyes protect themselves. Having dry eyes can cause other problems. Treatments can include eye drops or probes into the glands.
Meibomian gland dysfunction (MGD) happens when oil-secreting glands in your eyelids don’t secrete the quantity or quality of oil you need to prevent your eyes from drying out. MGD is a very common cause of dry eye syndrome.
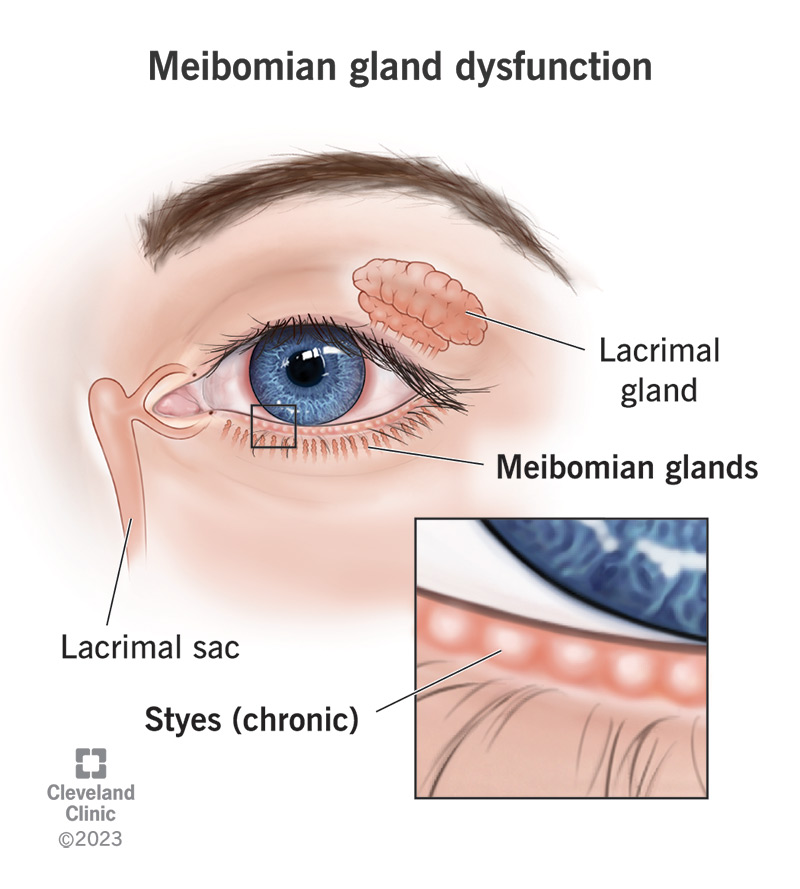
The meibomian glands are the parts in your eye that produce this necessary oil. This oil (meibum) makes up the oily outside layer of the tear film. There’s also a watery layer in the middle and a mucus layer inside.
MGD can be something you’re born with (congenital) or something that happens over time (acquired). It can happen to both older and younger people.
Most often, the glands fill up and oil can’t get out. The name for this is obstructive MGD.
Meibomian gland dysfunction is common. An estimated 35.8% of the people in the world have MGD. In the U.S., one estimate is that 70% of people over age 60 have MGD.
The condition is more common in people assigned male at birth (AMAB) than in people assigned female at birth (AFAB). The rates of MGD can vary among different ethnic groups. For instance, the rates are higher among people of Asian descent than among people who are white.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Some people with meibomian gland dysfunction don’t have symptoms. If you do have symptoms of MGD, they can include:
Meibomian gland dysfunction happens when the glands become blocked. Another factor is the quality of the oil the glands secrete. Certain medications, including glaucoma treatments, retinoids, estrogen for hormone replacement therapy and drugs that decrease androgen levels are potential causes.
Risk factors are things that may increase your chances of getting or having a condition. The risk factors for MGD include:
You may be more likely to have MGD if you also have certain conditions, including those that affect your immune system.
Advertisement
Meibomian gland dysfunction is serious because of its complications. It can lead to dry eye syndrome (dry eye disease), diseases of the eye surface and blepharitis (eyelid inflammation). MGD, if not treated, can make it more likely for you to have an infection or inflammation in general. MGD can also make these things more likely if you have eye surgery.
Untreated, MGD can result in damage to your cornea.
Your eye care provider will ask about your health and medical history. They’ll do a thorough eye exam. Your answers to questions about your eye health are part of the diagnosis. Looking at the inside of your eyelids may allow your provider to see signs of MGD.
Your provider may perform one or more of the following tests to diagnose MGD:
Advertisement
Treatment of meibomian gland dysfunction depends on many things, such as how advanced it is, why it’s happening and your overall health.
Your provider may suggest some home remedies, including:
Your provider may also recommend:
You won’t really have to recover from many of the treatments for MGD. In fact, your provider may recommend doing these consistently (like lid washes and taking supplements).
You may need some time to recover from any type of surgical procedure.
You can’t prevent meibomian gland dysfunction, but you may be able to reduce your risks in some cases.
You can’t change some risk factors (like your age, sex or ethnicity), but there are modifiable risk factors.
You may be able to reduce your risk by:
You may not even know you have MGD in the early stages, which makes it more important to get your eyes examined.
You may need to continue good eye hygiene practices throughout your life. If MGD is untreated, you could develop more serious complications, such as dry eye disease or issues with your cornea.
However, the outlook if you have MGD is typically good, even if you have to keep up with certain routines to manage the condition.
You should always see a provider if you have sight-related issues like eye pain or blurred vision.
If eye pain or vision loss comes on suddenly, go to an emergency room.
You may have many questions for your eye care provider, including:
MGD may be a lifelong issue for some people, especially if you have another condition that’s treated but not cured, like an immune system disorder.
You may be able to unclog a meibomian gland through self-care like warm compresses and massage. There are instrument- and machine-based options that are available to your provider.
These alternatives to self-care include things like:
A note from Cleveland Clinic
One of the reasons it’s so important to have regular eye exams is that your eye care provider can find issues before you even know you have them. This is true of meibomian gland dysfunction, which your provider can spot before you have symptoms. While the occasional episode of dry eye isn’t really a problem, continuous dryness is. Your meibomian glands are part of the way that your eyes protect themselves. It’s important to discover and treat meibomian gland dysfunction early to prevent complications.
Last reviewed on 01/30/2024.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy