A bile duct obstruction occurs when a blockage or narrowing in your bile ducts prevents bile from flowing as it should. Gallstones are the most common cause. Treatment involves identifying what’s causing the blockage and removing it to prevent serious complications.
A bile duct obstruction is a blockage in your bile ducts. Bile is a digestive juice that breaks down fats. It also contains a waste product called bilirubin.
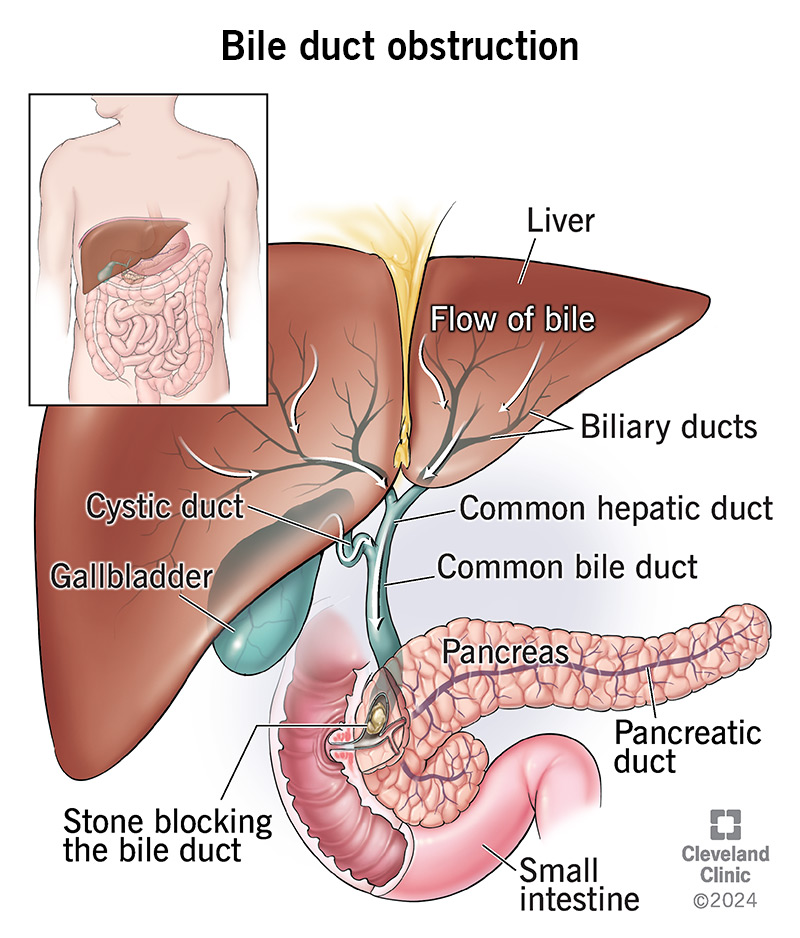
Your bile ducts are the tiny canals that allow bile to flow from your liver (where it’s made) to your gallbladder (where it’s stored) to your small intestine (where it helps with digestion). Bile ducts also help move bilirubin out of your liver.
Blockages in your bile ducts can slow or stop the flow of bile. This can cause bile to back up and collect in your liver. The results can feel painful and pose serious health risks without treatment.
Obstructions are the most common problem that can affect your bile ducts. Approximately 5 in 1,000 people develop gallstones that end up leading to an obstruction. Gallstones are hardened collections of bile. Gallstones are the most common cause of bile duct obstructions.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Symptoms are similar to those associated with gallstones and jaundice. Jaundice symptoms are a sign that there’s too much bilirubin in your bloodstream.
Signs to look out for include:
Causes of a bile duct obstruction include:
Bile duct strictures can result from a range of conditions (both malignant and benign). They can happen when there’s scarring after a medical procedure, like gallbladder removal surgery (cholecystectomy).
Causes of bile duct strictures that may lead to an obstruction include:
Advertisement
An obstruction can cause bile to build up in your liver. This can lead to severe inflammation and even life-threatening infections without treatment. It can also lead to permanent liver scarring (cirrhosis of the liver) that can lead to liver failure without proper management.
If the bile gets stuck in the part of the ducts near your gallbladder, you can get a gallbladder infection (cholecystitis).
Not having enough bile can also prevent your small intestine from digesting fats. This can lead to malnutrition.
Your provider will review your medical history, including your symptoms and medications. They’ll perform a physical exam to check for signs of an obstruction, like tenderness or swelling in your abdomen. You’ll need blood tests and imaging to confirm the obstruction and determine what caused it.
Blood tests can reveal signs of an obstruction. Tests your provider may order include:
You’ll need imaging tests if blood test results indicate a possible obstruction. You may need one or more of these imaging tests:
Advertisement
Treatment for a bile duct obstruction depends on how urgently you need care and what’s causing the blockage.
Treatments include:
You can’t always prevent a bile duct obstruction.
But you can reduce your risk of the biggest cause (gallstones) by reducing the foods you eat that are high in cholesterol. You can reduce your risk of several liver conditions that can lead to strictures by:
Your prognosis depends on what’s causing the obstruction. For example, prompt diagnosis and treatment can prevent complications from causes like gallstones. With treatment, many people recover completely.
Bile duct obstructions related to cancer and chronic liver disease may be more difficult to manage.
Everyone’s situation is different. Your healthcare provider will explain what you should expect from treatment based on what’s causing the blockage and how it’s impacting your health.
See your healthcare provider if you’re experiencing symptoms of a bile duct blockage. Many conditions can cause some of the common symptoms (like abdominal pain, nausea and vomiting). It’s important to confirm that the issue is a blockage sooner rather than later — before bile builds up and causes complications.
It can be, especially if backed-up bile leads to severe inflammation and infection. It’s best to see a provider when you first notice symptoms to prevent this from happening.
Your body depends on the free flow of bile through your bile ducts to aid in digestion and to remove bilirubin (a waste product) from your body. This is why it’s so important to fix any blockages. You need bile to arrive at your small intestine to break down fats. You need bilirubin to move out of your liver so it doesn’t cause complications, like liver disease or an infection. Your healthcare provider can discuss best options for removing a blockage if you have one.
Last reviewed on 01/30/2024.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy