Chronic obstructive pulmonary disease (COPD) refers to a group of diseases that includes chronic bronchitis and emphysema. Over time, COPD makes it harder to breathe. You can’t reverse lung damage, but lifestyle changes and medication changes can help you manage the symptoms.
COPD is an umbrella term for a range of progressive lung diseases. Chronic bronchitis and emphysema can both result in COPD. A COPD diagnosis means you may have one of these lung-damaging diseases or symptoms of both. COPD can progress gradually, making it harder to breathe over time.
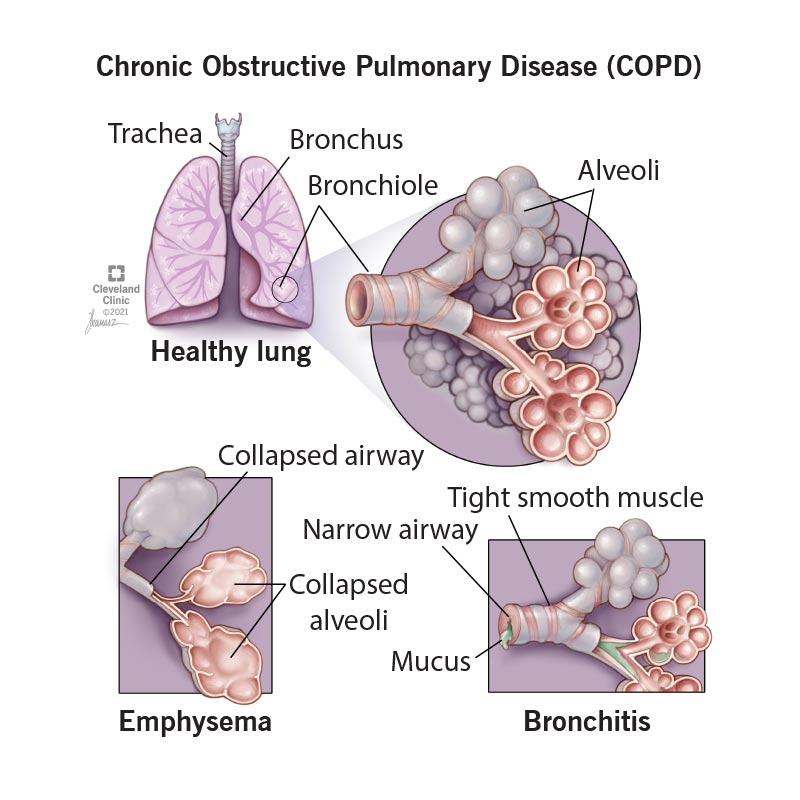
Chronic bronchitis irritates your bronchial tubes, which carry air to and from your lungs. In response, the tubes swell and mucus (phlegm or “snot”) builds up along the lining. The buildup narrows the tube’s opening, making it hard to get air into and out of your lungs.
Small, hair-like structures on the inside of your bronchial tubes (called cilia) normally move mucus out of your airways. But the irritation from chronic bronchitis and/or smoking damages them. The damaged cilia can’t help clear mucus.
Emphysema is the breakdown of the walls of the tiny air sacs (alveoli) at the end of the bronchial tubes, in the “bottom” of your lung. Your lung is like an upside-down tree. The trunk is the windpipe or “trachea,” the branches are the “bronchi,” and the leaves are the air sacs or “alveoli.”
The air sacs play a crucial role in transferring oxygen into your blood and carbon dioxide out. The damage caused by emphysema destroys the walls of the air sacs, making it hard to get a full breath.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Asthma and COPD are similar in many ways, including similar symptoms like shortness of breath and blocked airflow. However, COPD is chronic and progressive. Asthma is often set off by allergens. COPD’s main cause is smoking.
People with asthma don’t automatically develop COPD. People with COPD don’t always have asthma. However, it’s possible to have both of these respiratory conditions. If you do have both, you need to treat both.
Statistics put the number of Americans diagnosed with COPD at about 15 million people in 2020 with another 12 million not yet diagnosed.
Advertisement
The primary, or main, cause of COPD is smoking. But not all smokers develop the disease. You may be at higher risk if you:
Smoking tobacco causes up to 90% of COPD cases. Other causes include:
Tobacco smoke irritates airways, triggering inflammation (irritation and swelling) that narrows the airways. Smoke also damages cilia so they can’t do their job of removing mucus and trapped particles from the airways.
AAT (alpha-1 antitrypsin deficiency) is an uncommon, inherited disorder that can lead to emphysema. Alpha-1 antitrypsin is an enzyme that helps protect your lungs from the damaging effects of inflammation. When you have AAT deficiency, you don’t produce enough of alpha-1 antitrypsin. Your lungs are more likely to become damaged from exposure to irritating substances like smoke and dust. It’s not possible to distinguish COPD related to alpha-1 antitrypsin deficiency from common COPD. Therefore, all people with COPD should get screened for AAT deficiency with a blood test.
Advertisement
If you’re having any of the signs or symptoms of COPD, don't wait for your next appointment to call your provider. Report these symptoms promptly, even if you don't feel sick. Don't wait for symptoms to become so severe that you need to seek emergency care. If you notice your symptoms early, your provider might change your treatment or medications to relieve your symptoms. (Never change or stop taking your medications without first talking to your healthcare provider.)
Note: Remember that warning signs or symptoms might be the same or different from one flare-up to another.
Talk to your provider on the phone within 24 hours if you have these changes in your health:
Examples include:
Examples include:
These include:
To assess your lungs and overall health, your healthcare provider will take your medical history, perform a physical exam and order some tests, like breathing tests.
To diagnose COPD, your provider will ask questions like:
To help with the diagnosis, your provider will do a physical exam that includes:
Providers use a simple test called spirometry to see how well your lungs work. For this test, you blow air into a tube attached to a machine. This lung function test measures how much air you can breathe out and how fast you can do it.
Your provider may also want to run a few other tests, such as:
COPD can gradually get worse. How fast it progresses from mild to severe varies from person to person.
The first sign of COPD is often feeling out of breath with light exercises, like walking up stairs. Because it’s easy to blame this symptom on being out of shape or getting older, many people don’t realize they have COPD. Another sign is a phlegmy cough (a cough with mucus) that’s often particularly troublesome in the morning. These are early warning signs of COPD.
In general, shortness of breath is more evident with more advanced COPD. You may develop shortness of breath even during everyday activities. Also, exacerbations of COPD — times when you experience increased phlegm, discoloration of phlegm, and more shortness of breath — are generally more common in higher stages of COPD. You also become prone to lung infections like bronchitis and pneumonia.
When COPD becomes severe, almost everything you do can cause shortness of breath. This limits your mobility. You may need supplemental oxygen from a portable tank.
COPD treatment focuses on relieving symptoms, such as coughing and breathing problems, and avoiding respiratory infections. Your provider may recommend:
For severe COPD, your provider may suggest you consider a clinical trial (tests of new treatments) or lung surgery if you’re a candidate.
Not smoking is the best thing you can do to avoid developing COPD. If you’d like to quit, smoking cessation programs can help you. Also, avoid any environment that has poor air quality — air that has particles like dust, smoke, gases and fumes.
People with COPD have difficulty clearing their lungs of bacteria, dusts and other pollutants in the air. This makes them at risk for lung infections that may cause further damage to the lungs.
Therefore, it is important to watch for signs of infection and follow these tips to help prevent infections. You probably won’t be able to avoid infections entirely, but these tips will help you prevent infections as much as possible.
While you can treat most infections successfully, you must be able to recognize an infection's immediate symptoms for proper and effective care. These may include:
If you have any of these symptoms, contact your healthcare provider right away, even if you don’t feel sick.
There are things you can do to help prevent infections, including the following items.
Frequently wash your hands with soap and warm water, especially before:
Wash your hands thoroughly after:
It is also good to carry waterless hand sanitizers with you to use when necessary.
If visitors have cold or flu symptoms, ask them not to visit until they are feeling well.
COPD progresses at a different rate for every person. Once it progresses, you can’t reverse the lung damage from COPD but, by following a healthy lifestyle and getting treatment as early as possible, you can manage symptoms and feel much better.
Life expectancy for someone with COPD varies from person to person. It depends on how early your provider finds the disease, your general health (including other diseases you might have), and how you manage your treatment. Some people live quite a long time after diagnosis. Other people, with more severe disease, don’t fare as well.
Call your provider if you experience any of the warning signs of an infection. Also, call your provider if you have any symptoms that cause concern.
You can take several steps to make breathing easier and slow the progression of the disease:
The lungs of people with COPD are sensitive to certain substances in the air, such as cigarette smoke, exhaust fumes, strong perfumes, cleaning products, paint/varnish, dust, pollen, pet dander and air pollution. Extreme cold or hot weather conditions can also irritate your lungs.
You can avoid some of these irritants by:
A note from Cleveland Clinic
Chronic obstructive pulmonary disease (COPD) causes lung damage that you can’t reverse. However, you can learn to manage symptoms. You’ll breathe easier if you take the necessary steps to support your lung capacity and fight lung irritation. By getting treatment early, you’ll have the best chance of continuing to do the things you love.
Last reviewed on 05/17/2022.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy