Croup is a very contagious respiratory infection that mostly affects babies and young children. The condition causes swelling of your child’s voice box (larynx) and windpipe (trachea), which leads to symptoms including a distinctive barking cough and raspy breathing. Croup is usually mild but symptoms can become severe and life-threatening.
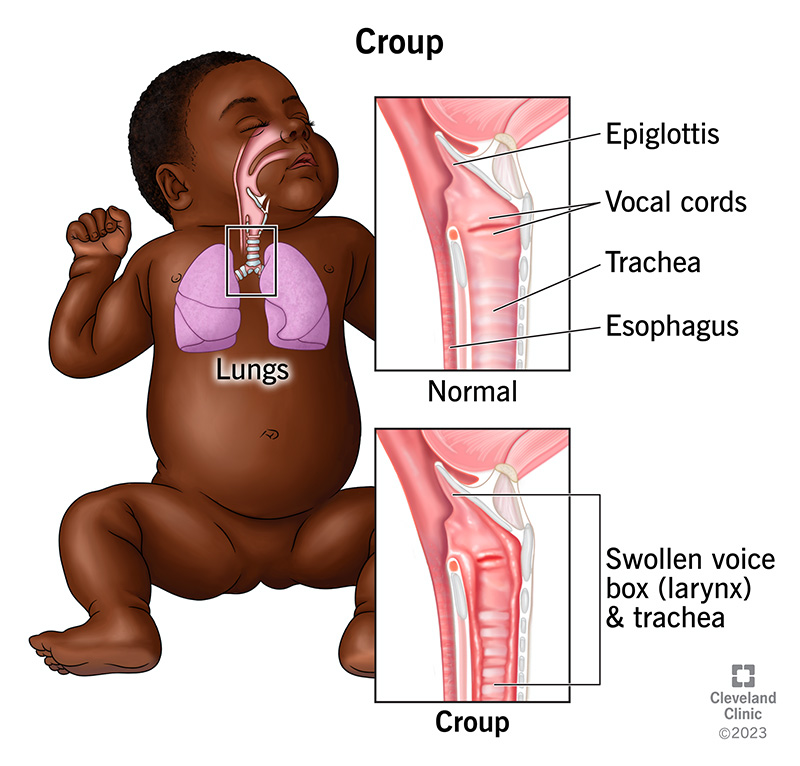
Croup (laryngotracheobronchitis) is a respiratory infection that affects young children. Viral infections are the most common cause of the condition. Croup causes swelling of your child’s voice box (larynx) and windpipe (trachea). This swelling causes the airway below their vocal cords to narrow, which makes their breathing noisy and difficult.
Croup in babies is most common, along with children younger than 3 years old. As children get older, croup isn’t seen as often. This is because their windpipes get larger and swelling is less likely to get in the way of their breathing.
Croup causes a distinctive cough that may sound similar to the call of a seal. The condition is usually mild but symptoms can become severe and life-threatening.
RSV (respiratory syncytial virus) and croup are both respiratory illnesses that can affect babies and young children. RSV is a viral infection that can affect both children and adults. It causes coughing, sneezing and other cold-like symptoms.
While RSV is its own illness, the respiratory syncytial virus is also one of the viruses that can lead to croup.
Whooping cough (pertussis) and croup are both respiratory infections that can affect babies and children. Both conditions cause a distinctive cough, although the sound of whooping cough is a more high-pitched gasping or “whooping” noise.
Whooping cough is a bacterial infection whereas a viral infection usually causes croup. Therefore, no vaccines can prevent croup and antibiotics can’t treat it. (Antibiotics can’t kill viruses.) There’s a vaccine to prevent whooping cough, but it doesn’t go away quickly on its own as croup usually does.
Croup affects about 3% of U.S. children every year. The condition accounts for 7% of all hospitalizations in children younger than 5 years old. It’s more common in boys and children assigned male at birth (AMAB) than girls and children assigned female at birth (AFAB). Healthcare providers define about 85% of croup cases as mild. They consider less than 1% of cases severe.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The croup cough sounds like a harsh “barking” sound. This is the most common symptom of croup. Your child may also have stridor, which is a raspy, vibrating sound that occurs when your child is breathing in.
Croup is typically mild and lasts less than one week, but symptoms can get more severe. Symptoms normally start slowly and may begin with a runny or stuffy nose. Over the next 12 to 48 hours, symptoms can worsen and the barking cough may start. Symptoms are usually worse at night.
Other mild croup symptoms include:
Symptoms of moderate to severe croup may include:
Advertisement
The most common cause of croup is a viral infection. Croup viruses include parainfluenza, influenza, respiratory syncytial virus (RSV), measles and adenovirus. Viral croup causes your child’s upper airways to swell, making it difficult for them to breathe. However, these viruses are common and most children with viral infections don’t develop croup. Rarely, bacteria can complicate the viral infection and make it more difficult to breathe.
Yes, croup is highly contagious because the viruses that lead to the condition are easily spreadable.
The viruses that cause croup spread easily through the air. When someone with a viral or bacterial infection that can cause croup sneezes or coughs, they send respiratory droplets containing croup-causing germs into the air. When your child breathes in these droplets, they can catch an illness that’ll cause croup. Your child can also get croup by touching objects contaminated by germs that can cause croup.
Your child is contagious for three days after their symptoms first appeared or until their fever is gone. You should keep your child home from school until 24 hours have passed without a fever and without using fever-reducing medication.
Most cases of croup are mild and you can treat them at home. Complications of croup are rare. Less than 5% of children with croup need in-hospital care. Your child’s condition may lead to hospitalization if they:
Advertisement
You can usually tell if your child has croup based on their signs and symptoms. The most common symptoms are a barking cough and stridor. This condition is especially widespread in the fall and winter months. If your child’s condition is severe, a healthcare provider may order X-rays and laboratory tests, but this is rare.
Croup treatment depends on the severity of your child’s condition and the risk of it rapidly worsening. If your child has a history of respiratory problems or was born prematurely, that may also affect the treatment approach.
You can usually treat mild croup at home. Home treatment includes using a cool mist humidifier to help soothe dry and irritated airways. You can also sit with your child in a bathroom filled with steam generated from hot water running in the shower. (Don’t sit in the shower or let your child near the hot water.) If your child’s condition doesn’t improve with mist treatment, you should contact their healthcare provider.
Other croup home remedies include:
You may wish to sleep in the same room as your child so you’re there if they start to have trouble breathing.
For moderate to severe croup, you should take your child to the nearest urgent care center or emergency room (ER). Severe croup can be life-threatening, and you shouldn’t delay taking your child in. Treatment for moderate to severe croup will vary based on your child’s symptoms. Croup treatments may include:
If you take your child to their provider’s office or the emergency room, their provider will give them a glucocorticoid and a nebulized breathing treatment (epinephrine).
Glucocorticoids are a type of steroid that decreases the swelling of your child’s voice box (larynx), typically within six hours of the first dose. For a child with mild croup, glucocorticoids may reduce the need for a repeat visit to their provider’s office or the emergency room.
The glucocorticoids healthcare providers use most often are dexamethasone and prednisolone. Your child will usually only need one dose taken by mouth (orally). If your child is vomiting or can’t keep the medicine down, their provider can also give dexamethasone intravenously (IV) or through an intramuscular (IM) injection.
Your child will receive epinephrine as an inhaled mist (nebulizer). This also reduces the swelling in your child’s airways and usually starts working within 10 minutes. Epinephrine works for two hours or less, and your child may receive this treatment every 15 to 20 minutes for severe symptoms.
Serious side effects of epinephrine are rare. However, side effects could include a rapid heartbeat (tachycardia). A healthcare provider will monitor your child for three to four hours after their last dose to ensure symptoms of airway blockage don’t return.
Glucocorticoids usually start working within six hours of the first dose. Epinephrine typically begins working faster than glucocorticoids.
Croup can spread by physical contact or through the air. To help prevent its spread:
Croup can be mild, moderate or severe, depending on how difficult it is for your child to pull air into their lungs. The size (diameter) of their windpipe and the amount of narrowing due to the swelling determine the severity of your child’s condition. In addition, your child’s condition may become more severe if they become upset.
A child with mild croup may have a barking cough and stridor. Symptoms can worsen throughout your child’s illness, especially during the evening hours. So it’s important to keep an eye on their breathing, but you can usually treat their condition at home.
A child with moderate croup may have stridor along with retractions (sucking in the skin around their ribs and the top of their breastbone). They may also be slightly agitated or disoriented and may have moderate trouble breathing. You should take your child to see a healthcare provider for treatment.
A child with severe croup has stridor and retractions. They may also be agitated, anxious or fatigued. Cyanosis (blue-tinged skin) is common. Severe croup is a life-threatening condition. Take your child to the emergency room immediately.
Symptoms of croup usually clear up in most children within two days. However, symptoms can persist for up to one week.
Croup is very contagious. Your child should stay home from school until after their fever is gone.
You should call your child’s healthcare provider if:
If your child develops symptoms of severe or worsening croup, seek immediate medical attention. These symptoms include:
If your child keeps getting croup, it may be a sign they have a narrowing in their airway and that they’re at a higher likelihood to be affected by the infection. Your child may have been born with the narrowing or it may have developed after birth. If croup returns (recurs) repeatedly, your child’s provider may refer them to a specialist such as an otolaryngologist (ear, nose and throat doctor) or a pulmonologist (breathing and lung disease doctor).
Adults can get croup, but it’s rare. The reason babies and young children get croup is because their windpipes (tracheas) are narrower and not fully developed. As children get older, their windpipes get larger and fully develop, so any swelling is less likely to affect breathing. Adults have larger airways, so croup doesn’t typically affect them. When adults do get croup, their symptoms are usually worse and they may need more aggressive treatment.
A note from Cleveland Clinic
Croup is a very contagious respiratory infection that affects babies and young children. You’ll know it’s croup because of the distinctive barking cough your child develops. While most cases of croup are mild, the condition can worsen quickly, become severe and prevent your child from breathing properly. If your child’s croup isn’t improving, contact their healthcare provider for evaluation and treatment.
Last reviewed on 05/03/2023.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy