Appendicitis occurs when your appendix gets clogged, infected and inflamed. Your appendix is a small, tube-shaped organ attached to your large intestine. Nobody knows what its purpose is — but we do know that appendicitis is serious. The standard treatment is surgery to remove your appendix.
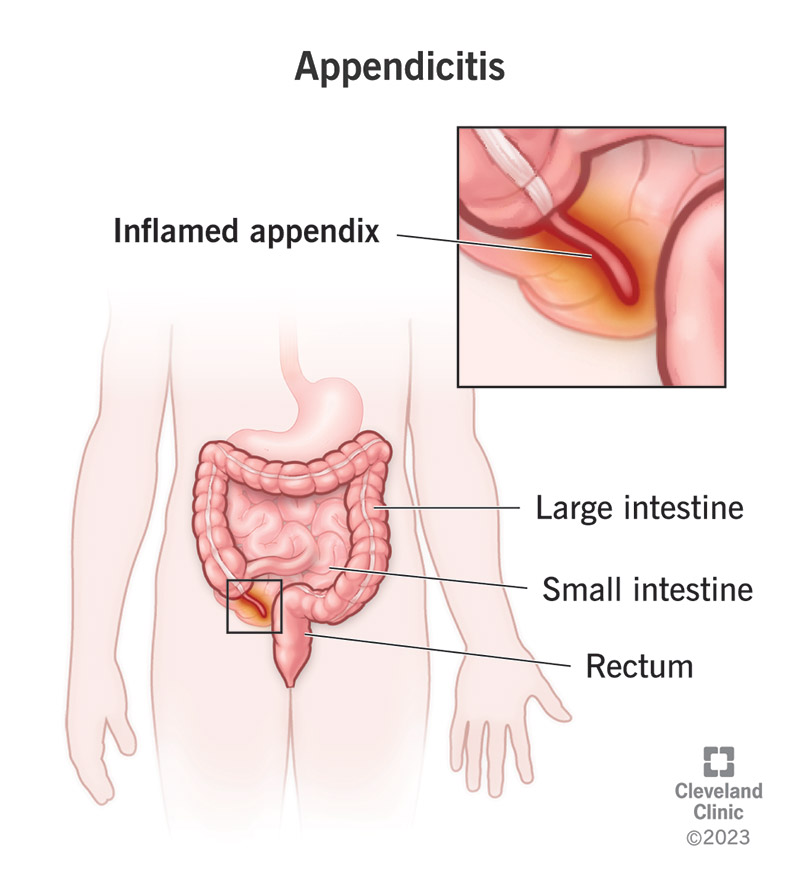
Appendicitis is an inflamed appendix. It can cause acute (sudden, intense) pain in your lower abdomen. Your appendix is a small, tubular pouch, about the size of a finger, that protrudes from the lower right end of your large intestine. Poop (feces) moving through your large intestine can block or infect your appendix, leading to inflammation. Inflammation causes your appendix to swell, and when it swells, it can burst.
A burst appendix is a medical emergency. It spreads bacteria from inside your bowels throughout your abdominal cavity. This infection (peritonitis) can then spread to your bloodstream, which can lead to life-threatening complications (sepsis). Because of this risk, the standard treatment for appendicitis is to remove your appendix (appendectomy). Your appendix isn’t an essential organ, and you won’t miss it.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Appendicitis is almost always an acute condition, which means it begins suddenly and worsens quickly. Most of what we know about appendicitis refers to acute appendicitis, which is very common. Chronic appendicitis is a rare condition that we don’t know as much about. It appears to occur when something irritates your appendix in an on-and-off sort of way over a long period, but it never gets worse.
Chronic appendicitis may go unrecognized because the symptoms don’t escalate the way they do in acute appendicitis. But any type of appendicitis is serious. If you have chronic abdominal pain and you don’t know what causes it, it’s important to see a healthcare provider about it. Chronic appendicitis may worsen or become acute at any time. Because of this risk, healthcare providers treat it the same way.
Acute appendicitis is common, especially between the ages of 10 and 30. Appendicitis in children is most common during the teen years, but younger children also get it. In the U.S., about 5% of the population will get acute appendicitis in their lifetime. It’s the leading cause of abdominal pain leading to emergency abdominal surgery. Chronic appendicitis occurs in approximately 1% of the population.
Advertisement
The most common symptoms of appendicitis are abdominal pain, nausea and loss of appetite. There’s a typical way these symptoms may present that can make it easier to recognize appendicitis. But unfortunately, only about half of people with appendicitis have the classic presentation of symptoms. Kids, elderly adults and pregnant people may be less likely to present with typical symptoms.
In the typical presentation, abdominal pain begins in the middle of your abdomen, around your belly button. It may hover or may come and go for several hours. Eventually, the pain intensifies, and nausea and vomiting develop. Several hours later, the nausea passes, and the pain shifts to your lower right abdomen, where your appendix is. The pain becomes more focused and continues to worsen.
Additional symptoms may develop later in some people. These can include:
If you suspect appendicitis, you should always have a healthcare provider check for it. But if you’re looking for a sign, there are a few that healthcare providers use to check for appendicitis. Pain location can be a helpful clue, especially if it begins around your navel and then moves to your lower right abdomen in the typical fashion. But some people feel the pain elsewhere. Providers may look for:
Symptoms of appendicitis can resemble many other conditions. This is especially true for women and people assigned female at birth (AFAB). Your lower abdomen lies close to your pelvic cavity, and conditions affecting your pelvic organs may feel very similar to appendicitis. These organs include your urinary system and female reproductive system. Other lower abdominal organs may also be involved.
Some common conditions that might be easily confused with appendicitis include:
The size and location of your appendix make it easy for it to become clogged and infected. Your large intestine is home to many bacteria, and if too many become trapped in your appendix, they overgrow and cause an infection. Sometimes, appendicitis begins with an infection, and sometimes, the infection is secondary. Swelling in your appendix can reduce or close the opening and trap more bacteria inside.
Common causes of inflammation, swelling, obstruction and infection in your appendix include:
Other factors that could block the opening to your appendix include:
The theory of chronic appendicitis is that something causes mild inflammation on and off for a long time. It might be a chronic condition like inflammatory bowel disease or mild bacterial overgrowth. Or it might be an obstruction that moves in and out of the opening to your appendix. Chronic inflammation can lead to lymphoid hyperplasia or even scar tissue in your appendix if it lasts a very long time.
Having a family history of appendicitis does appear to raise your risk of developing it, though it’s not clear why. Appendicitis itself is not inherited, but genetics might be involved in some of its causes.
It’s not likely. However, severe physiological stress from critical illness can cause bowel ischemia, a temporary reduction of blood flow to your intestines. Ischemic colitis may rarely affect your appendix.
There have been rare reports of an undigested seed or nut getting stuck in the opening to the appendix and causing inflammation. In general, though, eating more fiber reduces your risk of appendicitis.
Advertisement
Appendicitis can quickly lead to very serious complications, which is why healthcare providers treat it as an emergency. Complications can progress in stages, though they don’t always happen in the same way. Complications (stages) can include:
A healthcare provider will ask you detailed questions about your pain and other symptoms. They’ll perform a gentle physical exam to check for physical signs of appendicitis, such as guarding, stiffening and pain in response to pressure. If you have the typical profile of symptoms, they may be able to diagnose you right away. If you don’t, they may need to order further tests to confirm appendicitis.
Appendicitis tests typically include blood tests and imaging tests. Blood tests can show signs of inflammation, such as a high white blood cell count or C-reactive protein count, and they can help identify an infection. Imaging tests, such as an abdominal ultrasound or a CT scan, can show if your appendix is swollen. A healthcare provider may order additional tests to rule out other conditions.
It’s possible but not likely. Appendicitis may spontaneously resolve if the cause suddenly goes away on its own. This might happen if an obstruction in your appendix gets unstuck and passes on through your intestine, or if an infection that was causing lymphoid hyperplasia in your appendix suddenly improves. But you shouldn’t assume this will happen or that it has happened, even if your pain has reduced.
Appendicitis is considered an emergency, so it’s treated in the emergency room. The standard treatment includes both medication and surgery, though in a small number of cases, medication might be enough.
Almost everyone will need antibiotics for appendicitis. Even if you didn’t have an infection to start with, appendicitis usually leads to one. Antibiotics are also a standard preventive treatment before surgery.
If you have a very early and mild case of appendicitis, your healthcare provider might take a wait-and-watch approach to see if your condition improves with antibiotics alone. You might prefer this approach if you have risk factors that make surgery less safe for you. However, healthcare providers rarely recommend it because appendicitis often returns when you don’t have your appendix removed.
You may also need medication for pain relief. You can have this through your IV. If you’re having surgery, you’ll have general anesthesia, so you won’t be conscious (awake) during the procedure.
Once you’ve been diagnosed with appendicitis, time is of the essence. Your appendix can rupture within 36 hours of your first symptoms. Surgeons will usually schedule your appendectomy within 24 hours of your diagnosis. Appendectomy is one of the most common surgical procedures performed worldwide. Surgeons can often perform it using minimally invasive methods, such as laparoscopic surgery.
Your surgeon will also treat any complications you have during your surgery. Complications may require open abdominal surgery to manage. After surgery, they’ll rinse your abdomen with a sterile solution.
There aren’t any side effects of having your appendix removed. Healthcare providers aren’t sure if your appendix has any function. If it does, it’s a small one. It may help make antibodies during childhood.
If you had a simple laparoscopic appendectomy, you might be able to go home the same day. If you had complications or open surgery, you might need to stay in the hospital a little longer. You might need pain relief during your first few days at home. Most people have fully recovered within six weeks.
With early recognition and treatment, the outlook is good. Most people recover quickly and completely. If you had complicated appendicitis, your recovery might take longer. You might need repeat treatments for infection that spread beyond your appendix. Appendicitis that’s treated with antibiotics alone has a return rate of 40%. Appendicitis that goes untreated has a mortality rate greater than 50%.
Appendix pain is always an emergency. Seek medical attention immediately if you have any signs or symptoms of appendicitis, including:
A note from Cleveland Clinic
You might never think about your appendix until one day it starts hurting. If that happens, there’s no time for pleasantries — that’s your cue to head to the hospital. Appendicitis is serious, but it’s common, and if you need emergency surgery for it, you’ll be in experienced hands. Once it’s over, you’ll never have to worry about appendicitis again.
Last reviewed on 05/09/2023.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy