A stroke is your brain’s equivalent of a heart attack, happening when there’s an issue with blood flow to part of your brain. This can happen when blood vessels are blocked or because of bleeding in your brain. Strokes are a life-threatening emergency, and immediate medical attention is critical to prevent permanent damage or death.
A stroke is a life-threatening condition that happens when part of your brain doesn’t have enough blood flow. This most commonly happens because of a blocked artery or bleeding in your brain. Without a steady supply of blood, the brain cells in that area start to die from a lack of oxygen.
IMPORTANT: A stroke is a life-threatening emergency condition where every second counts. If you or someone with you has symptoms of a stroke, IMMEDIATELY call 911 (or your local emergency services number). The quicker stroke is treated, the more likely you’ll recover without disability.
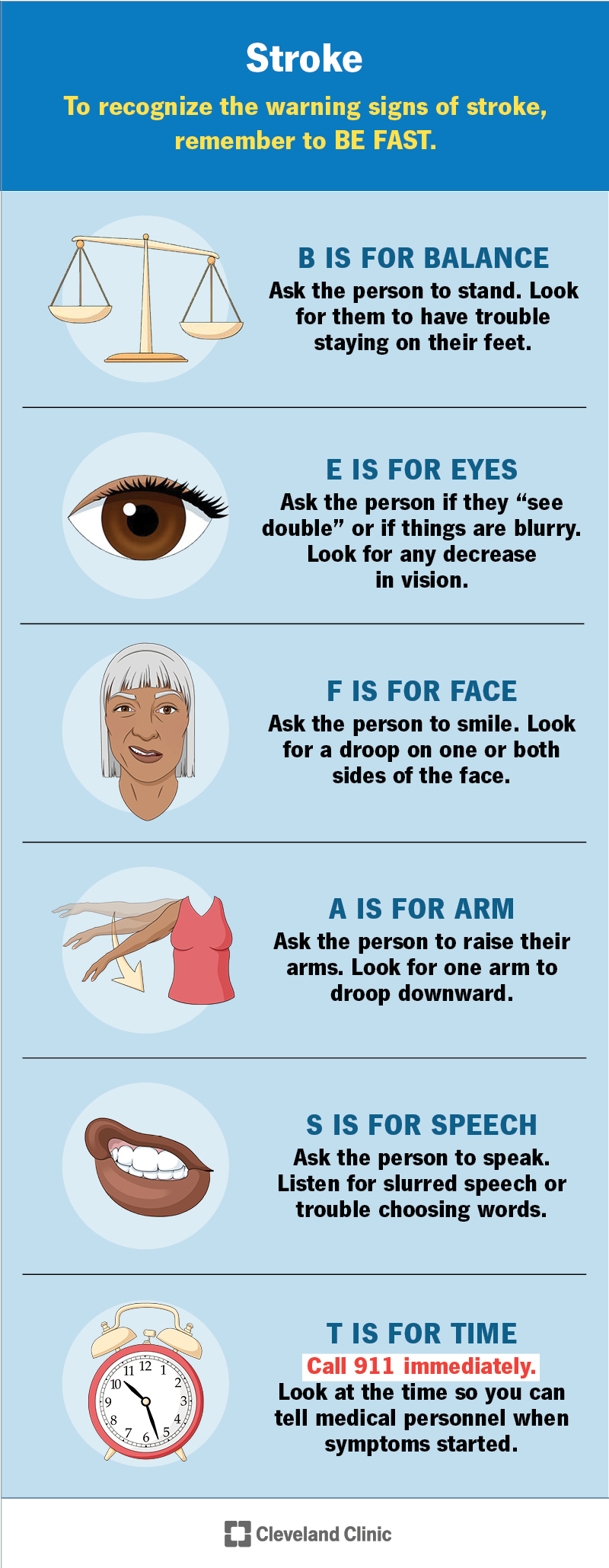
To recognize the warning signs of a stroke, remember to think BE FAST:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Anybody can have a stroke, from children to adults, but there are some people who have a greater risk than others. Strokes are more common later in life (about two-thirds of strokes happen in people over age 65).
There are also certain medical conditions that increase the risk of stroke, including high blood pressure (hypertension), high cholesterol (hyperlipidemia), Type 2 diabetes, and people who have a history of stroke, heart attack or irregular heart rhythms like atrial fibrillation.
Strokes are very common. Worldwide, strokes rank second among the top causes of death. In the United States, stroke is the fifth cause of death. Strokes are also a leading cause of disability worldwide.
Advertisement
Strokes are to your brain what a heart attack is to your heart. When you have a stroke, part of your brain loses its blood supply, which keeps that brain area from getting oxygen. Without oxygen, the affected brain cells become oxygen-starved and stop working properly.
If your brain cells go too long without oxygen, they’ll die. If enough brain cells in an area die, the damage becomes permanent, and you may lose the abilities that area once controlled. However, restoring blood flow may prevent that kind of damage or at least limit how severe it is. That’s why time is critical in treating a stroke.
There are two main ways that strokes can happen: ischemia and hemorrhage.
Ischemia (pronounced “iss-key-me-uh”) is when cells don’t get enough blood flow to supply them with oxygen. This usually happens because something blocks blood vessels in your brain, cutting off blood flow. Ischemic strokes are the most common and account for about 80% of all strokes.
Ischemic strokes usually happen in one of the following ways:
Hemorrhagic (pronounced “hem-or-aj-ick”) strokes cause bleeding in or around your brain. This happens in one of two ways:
Advertisement
Different areas of your brain control different abilities, so stroke symptoms depend on the affected area. An example of this is a stroke that affects Broca’s area, a part of your brain that controls how you use muscles in your face and mouth to speak. That’s why some people slur their words or have trouble speaking when they have a stroke.
The symptoms of stroke can involve one or more of the following:
A transient ischemic attack (TIA) — sometimes called a “mini-stroke” — is like a stroke, but the effects are temporary. These are often warning signs that a person has a very high risk of having a true stroke in the near future. Because of that, a person who has a TIA needs emergency medical care as soon as possible.
Ischemic strokes and hemorrhagic strokes can happen for many reasons. Ischemic strokes usually happen because of blood clots. These can happen for various reasons, such as:
Hemorrhagic strokes can happen for several reasons also, including:
Several other conditions and factors can contribute to a person’s stroke risk. These include:
Strokes aren’t contagious and you can’t pass them to or get them from other people.
A healthcare provider can diagnose a stroke using a combination of a neurological examination, diagnostic imaging and other tests. During a neurological examination, a provider will have you do certain tasks or answer questions. As you perform these tasks or answer these questions, the provider will look for telltale signs that show a problem with how part of your brain works.
The most common tests that happen when a healthcare provider suspects a stroke include:
Treating a stroke depends on many different factors. The most important factor in determining treatment is what kind of stroke a person has.
The medications and treatments used vary depending on the type of stroke and how soon a person receives treatment after the stroke. There are also long-term treatments for stroke. These happen in the days and months after emergency treatment deals with a stroke’s immediate threat.
Overall, your healthcare provider is the best person to tell you what kind of treatment(s) they recommend. They can tailor the information they provide to your specific case, including your medical history, personal circumstances and more.
Some examples of treatments for stroke are as follows:
| Ischemic stroke | Hemorrhagic stroke |
|---|---|
| Thrombolytic drugs (within three to four and a half hours). | Blood pressure management. |
| Thrombectomy (within 24 hours if there’s no significant brain damage). | Reversal of any medication that might increase bleeding. |
| Blood pressure management. | Use of medications or surgery to reduce pressure inside your skull. |
| Ischemic stroke | |
| Thrombolytic drugs (within three to four and a half hours). | |
| Hemorrhagic stroke | |
| Blood pressure management. | |
| Thrombectomy (within 24 hours if there’s no significant brain damage). | |
| Hemorrhagic stroke | |
| Reversal of any medication that might increase bleeding. | |
| Blood pressure management. | |
| Hemorrhagic stroke | |
| Use of medications or surgery to reduce pressure inside your skull. |
Thrombolytic drugs (their name is a combination of the Greek words “thrombus,” which means “clot,” and “lysis,” which means “loosening/dissolving”) are an option within the first three hours after stroke symptoms start. These medications dissolve existing clots. But they’re only an option within that three- to four-and-a-half hour time frame because after that, they increase the risk of dangerous bleeding complications.
In some cases, especially ones where thrombolytic drugs aren’t an option, a catheterization procedure known as mechanical thrombectomy is an option. Thrombectomy procedures are also time-sensitive, and the best window for these procedures is within 24 hours after symptoms start. This procedure involves inserting a catheter (tube-like) device into a major blood vessel and steering it up to the clot in your brain. Once there, the catheter has a tool at its tip that can remove the clot.
Because high blood pressure is usually why hemorrhagic strokes happen, lowering blood pressure is a key part of treating them. Lowering blood pressure limits bleeding and makes it easier for clotting to seal the damaged blood vessel.
Your body’s clotting ability relies on a process called hemostasis to stop bleeding and repair injuries. Supporting hemostasis involves infusion of medications or blood factors that make it easier for clotting to happen. Examples include vitamin K therapy, prothrombin or clotting factor infusions, and more. This treatment is most common with hemorrhagic strokes, and can help control bleeding (especially for people who take blood-thinning medications).
In some cases, surgery is necessary to relieve the pressure on your brain. This is especially true with subarachnoid hemorrhages, which are easier to reach because they’re on the outer surface of your brain.
There are several other ways that stroke treatment can happen. Some of these treatments are supportive directly, while others help avoid complications. Your healthcare provider can tell you more about these other treatments and which ones they recommend and why.
One of the most important ways to treat stroke is to help a person recover or adapt to the changes in their brain. That’s especially true when it comes to helping them regain abilities they had before the stroke. Stroke rehabilitation is a major part of recovery for most people who have a stroke. That rehabilitation can take many forms, including:
Other therapies are possible, depending on your case and circumstances. Your healthcare provider is the best person to tell you what kind of treatments can benefit you.
The side effects of stroke treatments depend greatly on the type of stroke, the treatments used, your medical history and more. Your healthcare provider can tell you more about the side effects you can or should expect and what you can do to manage or even prevent them.
A stroke is a life-threatening medical emergency, and you shouldn't try to self-diagnose or self-treat it. If you have — or someone with you has — stroke symptoms, you should immediately call 911 (or your local emergency services number). The longer it takes for stroke treatment to begin, the greater the risk of permanent brain damage or death.
The recovery time and how long it takes to feel better after treatment both depend on many factors. Your healthcare provider is the best person to tell you what you can expect and the likely timeline for your recovery.
There are many things you can do to reduce your risk of having a stroke. While this doesn’t mean you can prevent a stroke, it can lower your risk. Actions you can take include:
If you’re at risk for any kind of stroke, your healthcare provider may recommend changing your diet to avoid increases in blood pressure. Examples of this include:
If you have a stroke, many factors affect what you can expect, such as how big it is and where it is in your brain. There are also some key differences between ischemic and hemorrhagic strokes.
In general, the more severe an ischemic stroke is, the worse the damage. When brain damage is more severe, it’s more likely that you’ll lose certain abilities, at least temporarily. The faster you get medical attention for stroke symptoms, the better your chances that these effects are temporary or less severe.
These strokes usually cause much worse symptoms, especially when bleeding is more severe. The symptoms of hemorrhagic stroke tend to get worse quickly. People with hemorrhagic strokes tend to cause severe headaches, seizures and coma.
A stroke lasts as long as there’s a lack of blood flow to part of your brain. Without treatment, a stroke will continue until the brain cells in the affected areas of your brain die, causing permanent damage.
Even after you receive treatment for a stroke, it’s common for the effects to linger. Most people will take weeks or even months to recover. Most of the progress in recovery happens within the first six months to 18 months (approximately) after a stroke. Further progress is possible after that, but can be harder to achieve or take longer.
Your healthcare provider is the best person to tell you when you can return to your usual routine and activities. But it’s important not to push yourself too hard. Without enough time to recover, you could cause another stroke or other complications.
Strokes have the potential to cause death when they’re severe or if they go too long without treatment. However, the outlook can still vary widely depending on many factors. Those factors include where in your brain a stroke happens, how severe it is, your health history and more.
Your healthcare provider is the best person to tell you more about the outlook for your situation. The information they provide will be the most accurate and most relevant information that you can get.
If you have a stroke, your healthcare provider will talk with you about a plan for treatment and the timeline for your recovery. They may also prescribe medications, recommend therapy options and more. It’s important to talk with your healthcare provider about why they recommend these and what they can do for you.
Once you and your provider finalize the treatment plan, it’s very important that you follow it as closely as possible. Doing that will give you the best chance to maximize how much you recover. Other things you can do include:
You should see your healthcare provider as recommended. You should also see them if you notice any new symptoms affecting you, especially symptoms that might have a connection to your previous stroke. Even symptoms that don’t seem connected might be important, so don’t wait to discuss them with your healthcare provider.
You should call 911 (or your local emergency services number) and go to the nearest ER if you experience any symptoms of another stroke (see the FAST criteria at the top of this article to know the symptoms for which you should watch).
You should also go to the hospital if you experience any of the symptoms of dangerous complications that are common after a stroke. The most common complicating conditions include:
A note from Cleveland Clinic
A stroke is your brain’s version of a heart attack, making it a critical, life-threatening medical emergency. Strokes are also time-sensitive, and delays in care can lead to permanent brain damage and death. Strokes can be frightening for those who experience them or people nearby.
But the treatment options for stroke are expanding every day thanks to advances in our understanding of the brain, technological leaps in imaging and new medications. If you notice the symptoms of a stroke in yourself or someone you’re with, immediate medical attention is critical. The faster a person having a stroke gets medical care, the more likely the effects of the stroke will be limited or even reversible.
Last reviewed on 09/22/2022.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy