Lupus is an autoimmune disease that makes your immune system damage organs and tissue throughout your body. It causes inflammation that can affect your skin, joints, blood and organs like your kidneys, lungs and heart. A healthcare provider will help you find medications to manage your symptoms and reduce how often you experience flare-ups.
Lupus is a condition that causes inflammation throughout your body. It’s an autoimmune disease, which means your immune system damages your body instead of protecting it. You may experience symptoms throughout your body depending on where your autoimmune system damages tissue, including in your:
Visit a healthcare provider if you notice new pain, rashes or changes to your skin, hair or eyes.
Healthcare providers sometimes call lupus systemic lupus erythematosus (SLE). It’s the most common type of lupus, and means you have lupus throughout your body. Other types include:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
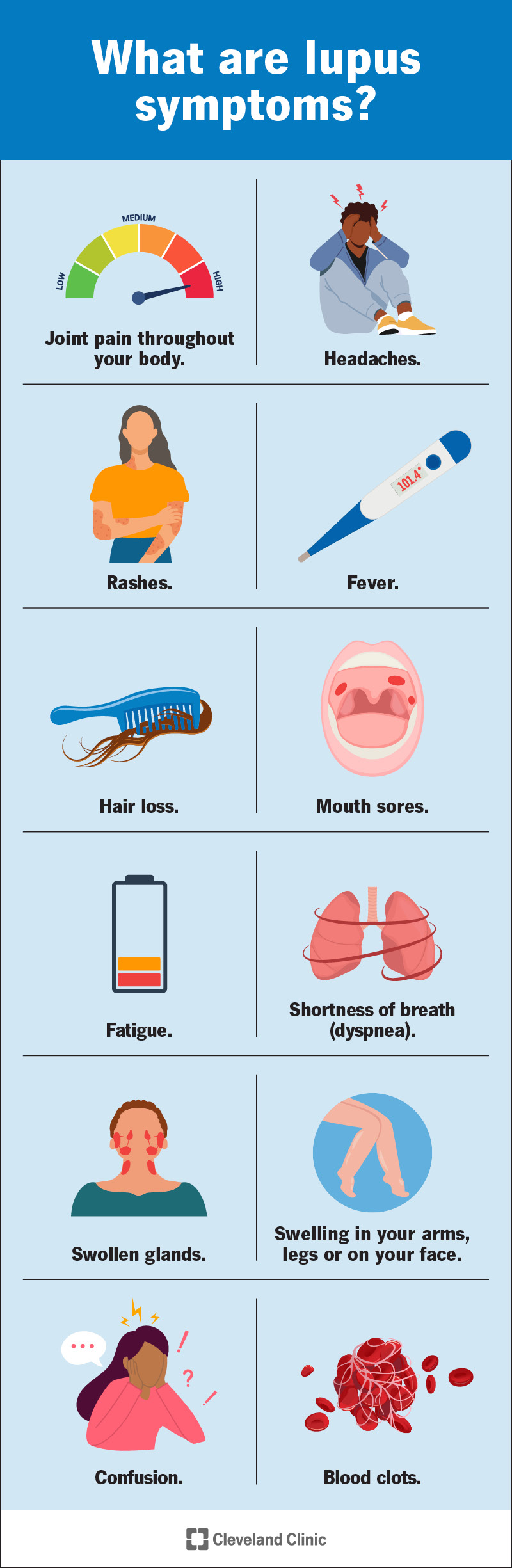
Lupus causes symptoms throughout your body, depending on which organs or systems it affects. Everyone experiences a different combination and severity of symptoms.
Lupus symptoms usually come and go in waves called flare-ups. During a flare-up, the symptoms can be severe enough to affect your daily routine. You might also have periods of remission when you have mild or no symptoms.
Symptoms usually develop slowly. You might notice one or two signs of lupus at first, and then more or different symptoms later on. The most common symptoms include:
Lupus can sometimes cause other health conditions or issues, including:
Experts don’t know for certain what causes lupus. Studies have found that certain factors about your health or where you live may trigger lupus:
Anyone can develop lupus, but some groups of people have a higher risk:
Advertisement
A healthcare provider will diagnose lupus with a physical exam and some tests. They’ll examine your symptoms and talk to you about what you’re experiencing. Tell your provider when you first noticed symptoms or changes in your body. Your provider will ask about your medical history, including conditions you may have now and how you’re treating or managing them.
Lupus can be tricky to diagnose because it can affect so many parts of your body and cause lots of different symptoms. Even small changes or issues that seem unusual for you can be a key. Don’t be afraid to tell your provider about anything you’ve felt or sensed — you know your body better than anyone.
There’s not one test that can confirm a lupus diagnosis. Diagnosing it is usually part of a differential diagnosis. This means your provider will probably use a few tests to determine what’s causing your symptoms before ruling out other conditions and diagnosing you with lupus. They might use:
Your healthcare provider will suggest treatments for lupus that manage your symptoms. The goal is minimizing damage to your organs and how much lupus affects your day-to-day life. Most people with lupus need a combination of medications to help them prevent flare-ups and lessen their symptom severity during one. You might need:
You might need other medications or treatments to manage specific lupus symptoms you have or other health conditions it’s causing. For example, you may need treatment for anemia, high blood pressure (hypertension) or osteoporosis if lupus causes those issues.
Advertisement
You can’t prevent lupus because experts aren’t sure what causes it. Talk to a healthcare provider about your risk if one of your biological parents has lupus.
You might be able to prevent and reduce lupus flare-ups by avoiding activities that trigger your symptoms, including:
Lupus is a lifelong (chronic) condition. You should expect to manage lupus symptoms for the rest of your life.
Lupus can be unpredictable, and the way it impacts you can change over time. You’ll need to regularly visit your healthcare provider so they can track changes in your symptoms.
You’ll probably work with a team of providers as you learn to live with lupus. Your primary care provider will suggest specialists who can help with specific issues or symptoms. You’ll probably need to visit a rheumatologist — a healthcare provider who specializes in diagnosing and treating autoimmune diseases. Which specialists you need to visit depends on which symptoms you have and how they affect your body.
There’s currently no cure for lupus. Your healthcare provider will help you find a combination of treatments to manage your symptoms and hopefully put lupus into remission (long periods of time with no symptoms or flare-ups).
Visit a healthcare provider as soon as you notice any new or changing symptoms. Even small shifts in what you’re feeling and experiencing can be important.
Talk to your provider if it feels like your treatments aren’t managing lupus symptoms as well as they used to. Tell your provider if you’re having flare-ups more often — or if the flare-ups cause more severe symptoms. They’ll help you adjust your treatments as needed.
Go to the emergency room or call 911 (or your local emergency services number) if you’re experiencing any of the following symptoms:
A note from Cleveland Clinic
Lupus can be a frustrating, tiring condition. Pain, inflammation and irritation throughout your body can be exhausting. But don’t forget to appreciate yourself. Living with a chronic condition is hard work, and you deserve credit for managing your symptoms every day. Ask your provider about mental health resources and support groups if you think talking to someone about how you’re feeling could help you.
Don’t be afraid to talk to your provider and ask questions. Even small changes in your symptoms or health can be a sign that lupus is affecting you differently. Remember, you’re the best judge of when something isn’t quite right in your body.
Last reviewed on 09/06/2023.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy