Attention-deficit/hyperactivity disorder (ADHD) is one of the most common childhood neurodevelopmental disorders. Children with ADHD often have difficulty with inattention, hyperactivity and impulsivity. Kids usually receive a diagnosis during childhood, and the condition often lasts into adulthood. However, effective treatment is available.
Attention-deficit/hyperactivity disorder (ADHD) is one of the most common and most studied neurodevelopmental disorders in children. “Neuro” means nerves. Scientists have discovered there are differences in the brains, nerve networks and neurotransmitters of people with ADHD.
ADHD is a long-term (chronic) brain condition that causes executive dysfunction, which means it disrupts a person’s ability to manage their own emotions, thoughts and actions. ADHD makes it difficult for people to:
Kids usually receive a diagnosis during childhood and the condition often lasts into adulthood. However, effective treatment is available. Left untreated, ADHD can cause serious, lifelong complications.
According to the Centers for Disease Control and Prevention, almost 11% of U.S. children between the ages of 2 and 17 have received an ADHD diagnosis. Worldwide, 7.2% of children have received an ADHD diagnosis.
Boys and children assigned male at birth (AMAB) receive an ADHD diagnosis more than twice as often as girls and children assigned female at birth (AFAB). But this doesn’t mean more boys and children AMAB have ADHD. It just means they present more often with hyperactive-type symptoms and are therefore easier to diagnose.
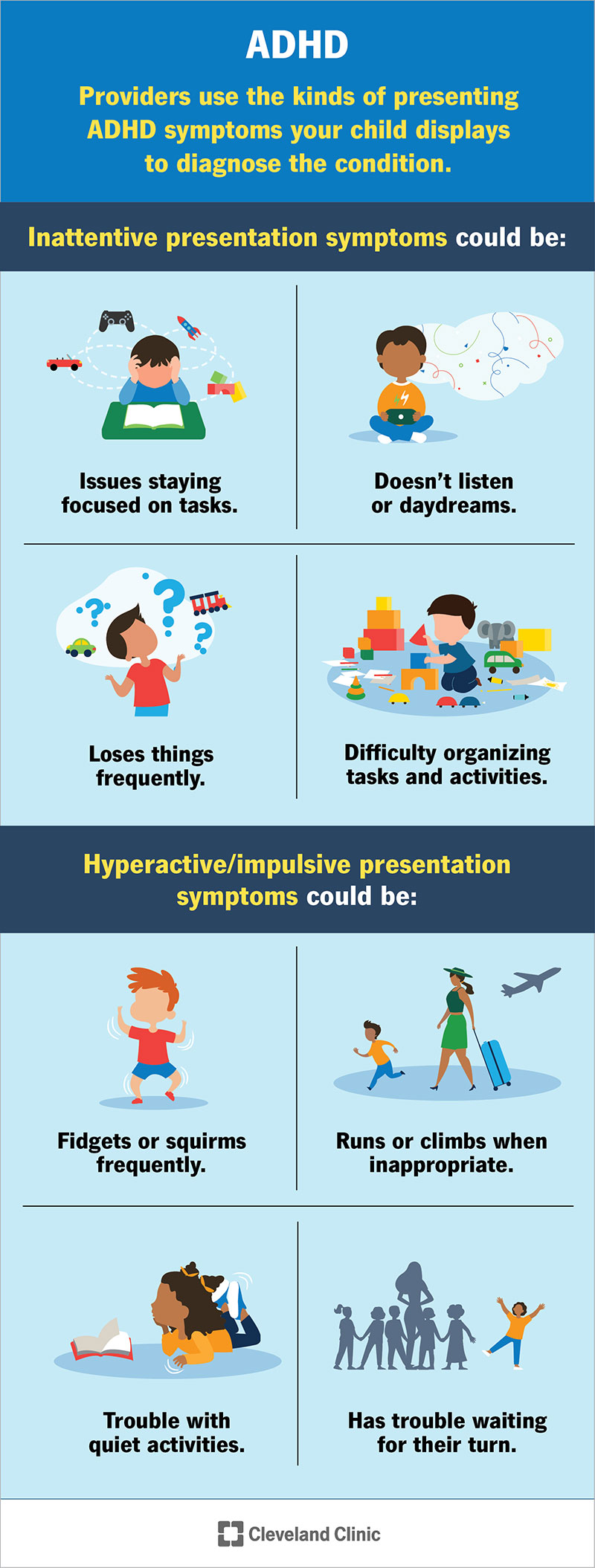
There are four different ways ADHD can present itself. Providers use the kinds of symptoms your child displays to diagnose the condition in one of these four ways.
Children with this presentation have inattentive ADHD only. Providers previously called this type attention-deficit disorder (ADD). Children with inattentive presentation mainly have difficulty focusing, organizing and staying on track, and have fewer hyperactivity/impulsivity symptoms.
Children with this presentation show issues with hyperactivity and impulsivity and may show less obvious trouble with paying attention. Hyperactivity means they may fidget, can’t sit still, have a lot of excess energy and are extremely talkative. Impulsivity means they may interrupt others and act without thinking it through first. This is the least common type and typically affects younger children.
Children with this presentation show at least six symptoms from both of the other types. Symptoms of inattentiveness and hyperactivity-impulsivity present equally. This type is what people most commonly associate with ADHD. About 70% of cases fall under this type.
In these cases, symptoms may be so severe that children clearly demonstrate dysfunction but don’t meet official symptom criteria for a diagnosis of ADHD inattentive, hyperactive/impulsive or combined type. In such cases, providers assign “unspecified ADHD” as the diagnosis.
Providers used to call the inattentive presentation type of ADHD “attention-deficit disorder (ADD).” In 1994, the American Psychiatric Association officially changed its name. Providers now call all forms of ADHD “attention-deficit/hyperactivity disorder” whether or not symptoms of hyperactivity are present. As described above, providers diagnose the different types based on the symptoms.
Although the name change happened decades ago, many people still refer to the condition as attention-deficit disorder (ADD). The difference between ADD and ADHD is the former doesn’t include symptoms of hyperactivity or impulsivity.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your child’s provider will make a diagnosis based on the presence and absence of certain symptoms. The symptoms must have interfered with functioning in at least two areas of life (such as school and home) and have occurred for at least the past six months.
Providers use the signs of ADHD to diagnose and determine the type of condition: inattentive, hyperactive/impulsive, combined or unspecified. The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition Text Revision (DSM-5-TR™) provides guidelines providers use to make diagnoses.
ADHD symptoms in kids with inattentive presentation include difficulty focusing, organizing and staying on task. According to the DSM-5-TR, a child with this type must display at least six of the following nine behaviors. (The behaviors must pose a problem in daily activity, at school and at home — not just from time to time, as most children engage in these behaviors.)
People with hyperactive/impulsive type display the following ADHD symptoms. According to the DSM-5-TR, a child must display at least six of the following nine behaviors. These must pose problems in daily activity.
People with combined type display behaviors from both the inattentive and hyperactive/impulsive categories. According to the DSM-5, children must display at least 12 of the total behaviors (at least six inattentive behaviors and six hyperactive/impulsive behaviors).
Scientists have identified differences in the brain structure and activity of people with ADHD. The frontal lobe is the front part of your brain, the part behind your forehead. The frontal lobe is responsible for planning, paying attention, making decisions and using language to moderate behavior. Researchers call this kind of activity directed attention. The brains of people with ADHD tend to reach their full maturity at a later time than those of neurotypical people.
People use directed attention to suspend automatic attention, a second kind of attention, which is very strong in people with ADHD. Directed attention, however, takes a lot of effort and is difficult to use. In a person with ADHD, directed attention skills tend to be weaker. Automatic attention is the kind of attention you use when you’re doing something that’s interesting or engaging. Directed attention is the kind of attention you use when you must do something that’s tiring or of low interest. (For example, in childhood, boring, repetitive tasks.)
In addition, nerve cells called neurons transmit signals in your brain. These signals travel through your brain in groups of neurons called networks. Scientists call the automatic attention network in your brain the default mode. They call the directed attention network in your brain the task-positive mode, or your brain’s executive network. Researchers have found major networks that work differently in people with ADHD. Neurotransmitters — chemicals that help transmit signals from one nerve cell to another — also play a role in ADHD.
Although researchers have discovered these brain differences, they don’t completely understand why they occur and lead to symptoms of ADHD. But current research shows that genetics plays a vital role. ADHD often runs in families — a child with ADHD has a 1 in 4 chance of having a parent with the condition.
Other possible causes and risk factors of ADHD may include:
The following aren’t causes of ADHD:
Advertisement
Without treatment, ADHD can potentially lead to a number of long-term complications. These complications may include:
If you’re worried that your child may have ADHD, the first step is to make an appointment with their healthcare provider. Your child’s pediatrician or another specialist can determine if your child has ADHD using a set of guidelines developed by the American Academy of Pediatrics. The guidelines are specifically for children ages 4 to 17. It’s hard to diagnose ADHD in children younger than 4 because they can change very quickly, and many kids at this age are naturally overactive or inattentive. It may also be harder to diagnose ADHD in teenagers due to other conditions they may have, such as depression or anxiety.
There’s no ADHD test to help diagnose the condition. Your child’s provider will take several steps and gather lots of information to help them make a diagnosis. The key factor is multiple people observing the behaviors associated with ADHD in different settings, such as at school and at home. A number of people will be involved in assessing your child’s behavior, including:
Based on this reported information, your child’s provider will look at how your child’s behavior compares to other children their age. Noting your child’s symptoms, they’ll also use guidelines found in the DSM-5-TR to help diagnose ADHD. The DSM-5-TR states that:
After they’ve evaluated your child and their symptoms, they can make a diagnosis along with the type of ADHD. A thorough assessment of behavior is critical (not just neuropsychological testing of attention), as many children who are quite bright may perform well in school even while showing inattentive symptoms.
ADHD affects about 4.2% of U.S. adults. But there are likely many more adults with undiagnosed ADHD. In some cases, it may be difficult to diagnose ADHD in adulthood due to other conditions such as depression and anxiety.
You may recognize the symptoms of ADHD in yourself during your child’s diagnosis. To get an ADHD diagnosis as an adult, you must have at least five of the symptoms associated with the condition. In addition, there must be evidence that the condition started during childhood. Several additional factors are involved in making a diagnosis, including:
Advertisement
The goal of ADHD treatment is to improve your child’s symptoms so they can function more effectively at home and school. For younger children (ages 4 and 5), providers recommend intervention for parents as the first line of treatment before medication is tried.
In most cases, the best ADHD treatment for older children, adolescents and adults includes a combination of behavioral therapy and ADHD medication.
For children younger than age 13, providers recommend parent training in behavior management. For adolescents, they recommend other types of behavioral therapy and training such as social skills training or executive function training. The goal of behavioral therapy is to learn or strengthen positive behaviors while eliminating unwanted or concerning behaviors. The goal of executive function training is to improve organizational skills and self-monitoring.
Medication can help people with ADHD manage their symptoms and the behaviors that cause issues with their friends, family and other contacts. The U.S. Food and Drug Administration has approved several different types of medications to treat ADHD in children as young as 6 years old.
Your child may need to try different medications and different doses before they find the right balance between the benefits and side effects.
Scientists believe genetics plays a major role in the development of ADHD. So, you can’t prevent the occurrence of the condition.
But there are certain risk factors you may be able to avoid. If you’re pregnant, avoid toxins and substances such as alcohol, tobacco and recreational drugs. This may reduce your risk, but researchers know little about ways to reduce the incidence and prevalence of ADHD.
The long-term outlook (prognosis) of ADHD depends on whether your child receives treatment. With behavior therapy and/or medication, most children go on to live healthy lives.
Without treatment, people with ADHD may experience poorer outcomes and lifelong complications. These may include:
People don’t outgrow ADHD, but some people learn to manage their symptoms effectively and may not meet the criteria for ADHD once they’ve reached adulthood. For some people, ADHD symptoms still affect their functioning — it’s a lifelong condition. However, many learn to manage it so that symptoms don’t impact their ability to function, allowing them to lead fulfilling lives.
Staying healthy is especially important for children with ADHD. In addition to behavioral therapy and medication, leading a healthy lifestyle can make it easier for your child to deal with their symptoms. Healthy behaviors include:
You may find the following strategies helpful for managing ADHD in the home.
ADHD stands for attention-deficit/hyperactivity disorder. The meaning of ADHD helps define the condition. Children with ADHD often have difficulties with inattention and hyperactivity, as well as impulsivity.
Almost all children have moments of daydreaming, misbehavior and/or distraction. But for children with ADHD, these moments are more than an occasional concern. The behaviors occur so frequently and at such an extreme level that they interfere with their ability to function effectively in daily activities.
No, ADHD isn’t on the autism spectrum. But autism spectrum disorder and ADHD are both neurodevelopmental disorders. They share some of the same symptoms. In addition, if your child has one of these disorders, their chances of having the other may increase.
Yes, the Americans with Disabilities Act (ADA) considers ADHD a developmental disability. The challenges the condition presents can make it difficult for your child to perform their daily activities and function efficiently at school. Therefore, your child may qualify for special education and/or modified instruction in school accommodations.
In addition, learning disabilities such as dyslexia and dyscalculia show a higher incidence in children with ADHD than in the neurotypical population. About 30% to 40% of children with ADHD also have a learning disability. Like those with ADHD, children with learning disabilities are eligible to receive special education services.
Yes, people with ADHD have many abilities and skills beyond those of people with neurotypical brains. Some companies deliberately hire people who are neurodivergent because of these advantages. These abilities and skills may include:
Girls and children assigned female at birth (AFAB) are just as likely as boys and children assigned male at birth (AMAB) to have ADHD. The condition often looks different in girls and children AFAB, but ADHD affects both sexes equally. Girls and children AFAB tend to show more inattentive symptoms in younger ages than boys and children AMAB, who show more hyperactive symptoms that are readily observable.
Despite widespread improvements in diagnosing the condition, some healthcare providers still work with outdated stereotypes that the condition affects boys and children AMAB more. Therefore, girls and children AFAB are more likely to go undiagnosed and less likely to receive treatment.
A note from Cleveland Clinic
Attention-deficit/hyperactivity disorder (ADHD) is a common, lifelong condition that affects people of all ages. Although it can affect your child’s behavior and attention, it’s treatable with therapy and medication. Behavioral treatments and support from friends, family and teachers (called social scaffolding) are important ways to help you manage your child’s condition. If you’re concerned your child may have ADHD, reach out to their healthcare provider. They can help you through the steps of getting a diagnosis and figuring out the right treatment plan for your child.
Last reviewed on 02/22/2023.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy