Irritable bowel syndrome, or IBS, causes uncomfortable or painful abdominal symptoms. Constipation, diarrhea, gas and bloating are all common symptoms of IBS. IBS doesn’t damage your digestive tract or raise your risk for colon cancer. You can often manage symptoms through medications, diet and lifestyle changes.
Irritable bowel syndrome (IBS) is a group of symptoms that affect your digestive system. It’s a common but uncomfortable gastrointestinal disease, or condition that affects your intestines.
People with IBS experience symptoms that include abdominal pain and cramps. With IBS, you may also have frequent diarrhea, constipation or both. IBS doesn’t cause tissue damage in your GI (gastrointestinal) tract or increase your risk of more serious conditions, like colon cancer. Instead, it’s a chronic (long-term) condition that most people can manage by changing their routines and what they eat, taking medications and receiving behavioral therapy.
Researchers categorize IBS based on how your stools (poop) look on the days when you’re having symptom flare-ups. Most people with IBS have normal bowel movements on some days and abnormal ones on others. The abnormal days define the kind of IBS you have.
The differences are important. Certain treatments only work for specific types of IBS.
It’s very common. Experts estimate that about 10% to 15% of adults in the United States have IBS. Only about 5% to 7% see a provider and receive a diagnosis.
It’s the most common disease that gastroenterologists (experts in GI diseases) diagnose.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
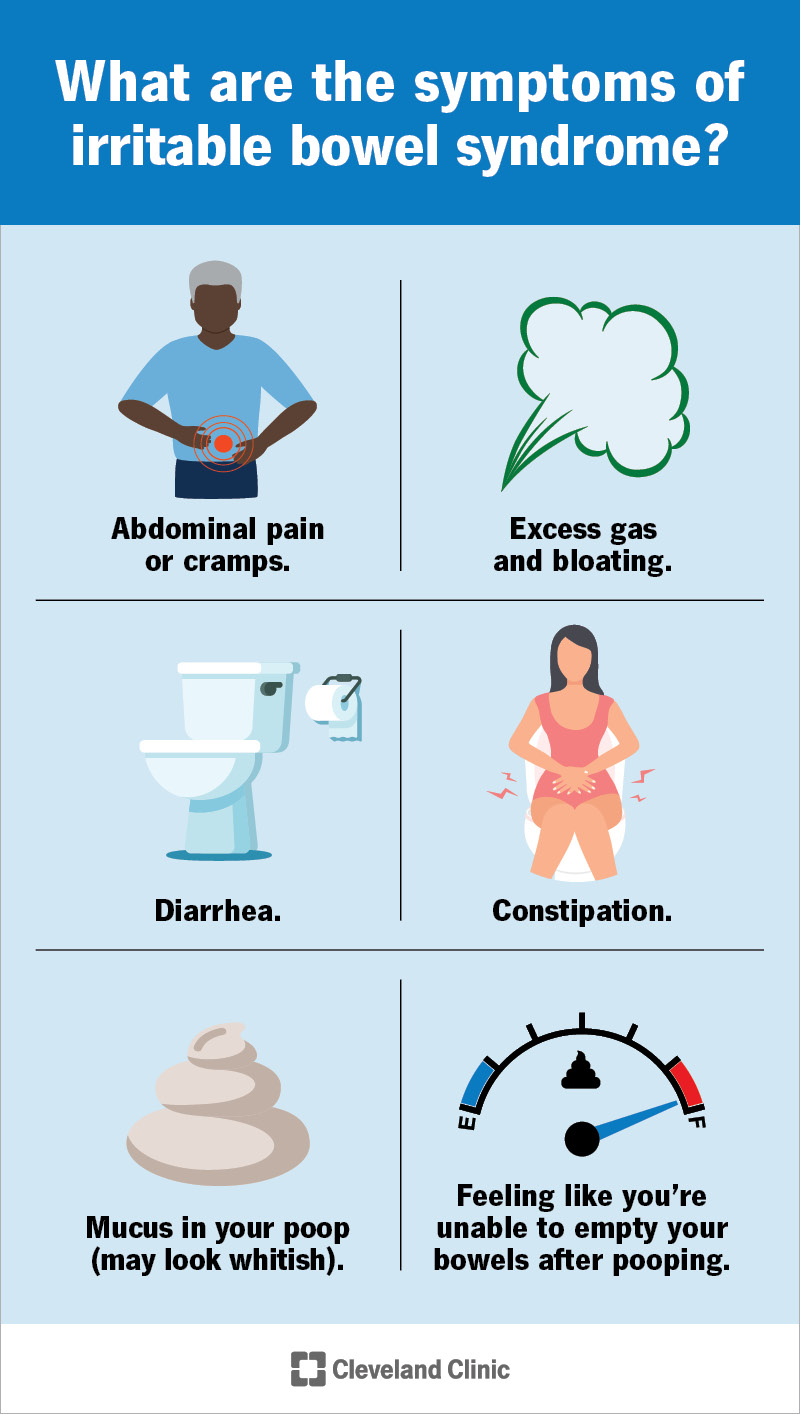
Symptoms of IBS can appear frequently. Or, they may occur during flare-ups. In other words, you don’t always experience symptoms. Instead, symptoms may go away (and you’ll have normal bowel movements). At other times, symptoms return.
Signs and symptoms of IBS include:
Researchers don’t know exactly what causes IBS, but they classify it as a neurogastrointestinal (GI) disorder. These conditions, also called disorders of the gut-brain interaction, have to do with problems with how your gut and brain coordinate to help your digestive system work.
Communication challenges between your brain and gut can cause:
Other potential causes of IBS include:
If you have IBS, you may have noticed that certain things trigger symptoms. A trigger doesn’t cause the condition itself, but it can cause or worsen a symptom flare-up. Common triggers include:
IBS most often occurs in people in their late teens to early 40s. People assigned female at birth (AFAB) are up to twice as likely to get diagnosed with IBS. Other risk factors include:
Many people with IBS also have other chronic pain conditions. Conditions associated with an increased risk of IBS include:
Advertisement
The first step in diagnosing IBS is a detailed medical history. Your provider will ask about your symptoms. They may ask:
Depending on your symptoms, you may need other tests to confirm a diagnosis. There isn’t a single test to diagnose IBS. Instead, your provider will determine if you have IBS by:
Most lab tests exclude other conditions that may be causing your symptoms, like an infection, food intolerance or a different digestive condition, like inflammatory bowel disease (IBD). Not everyone needs the same tests.
You may need imaging procedures to rule out conditions involving inflammation or abnormal growths in your GI tract.
No specific therapy works for everyone, but most people with IBS can find a treatment plan that works for them. Typical treatment options include changing the foods you eat and your routine. Medications can help, too. Behavioral health therapy may help.
Many of these treatments take time to work. They can help your symptoms, but your symptoms may not go away completely.
A dietitian can help you choose foods and modify eating/drinking habits to avoid symptom flare-ups. They may recommend that you:
Changing daily activities can help, too. Your provider may recommend that you:
Many people with IBS benefit from seeing a therapist. Therapy can help you get a handle on stress and conditions such as anxiety and depression that contribute to IBS. Some people find relief through:
Your healthcare provider may prescribe medications to provide symptom relief, including:
Although research into their effectiveness is ongoing, your provider may recommend probiotics. These “good bacteria” may help relieve IBS symptoms.
Medications specifically used to treat IBS include:
Advertisement
There isn’t a cure for IBS. But, most people manage symptoms by avoiding triggers and taking medications when necessary.
Since there’s no known cause for IBS, you can’t prevent or avoid it. If you have IBS, you can keep symptoms from flaring up by avoiding triggers.
No, IBS doesn’t put you at higher risk of developing conditions such as colitis, Crohn’s disease or colon cancer.
Living with IBS can be challenging because symptoms come and go throughout your life. Treatment often involves trial and error. But the good news is that nearly everyone with IBS can find a treatment that helps them over time.
Usually, changing the foods you eat and your activity levels improve symptoms with time. You may need some patience as you figure out your triggers and take steps to avoid them. Your symptoms may not completely disappear. But, after a few weeks or months, you should notice a significant improvement in how you feel.
See your provider if your symptoms continue for more than three months or if they’re getting worse. If you have symptoms less often, but they interfere with your life, it’s still a good idea to talk to your primary care provider.
Some symptoms may indicate a more serious problem. Contact your provider as soon as possible if you have common IBS symptoms alongside:
If you have IBS symptoms, ask your provider:
A note from Cleveland Clinic
IBS symptoms, like stomach pain, diarrhea, constipation and gas, are uncomfortable and can interfere with your life. But IBS is manageable. You can improve symptoms by changing what you eat and adjusting your daily habits to better handle triggers. If you have stomach symptoms that aren’t going away, talk to your healthcare provider. Together, you can find an IBS treatment plan that works for you.
Last reviewed on 11/16/2023.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy