A stomach ulcer occurs when gastric acid eats away at your protective stomach lining. The acid produces open sores that can bleed and cause stomach pain. Stomach ulcers are one kind of peptic ulcer disease. They’re common and treatable, but they should be taken seriously.
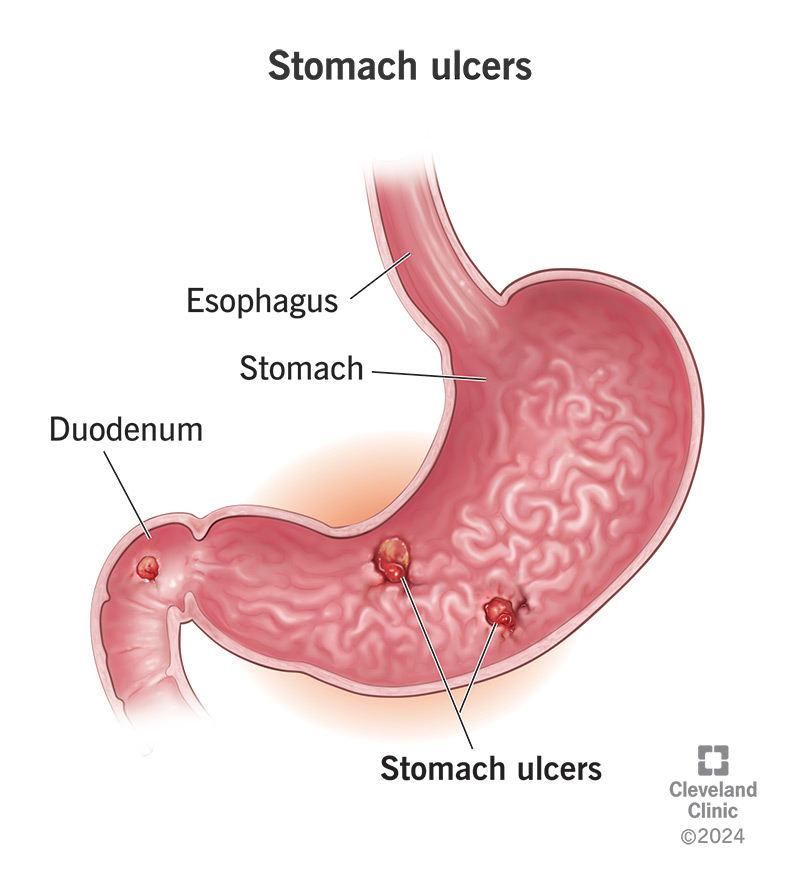
A stomach ulcer, also called a gastric ulcer, is an open sore that develops in your stomach lining. You can also get one in your duodenum, the first part of the small intestine that your stomach feeds into. Duodenal ulcers and stomach ulcers are both types of peptic ulcers. They’re named for pepsin, one of the digestive juices that are found in the stomach and that sometimes leak into the duodenum. These juices are a contributing factor in peptic ulcer disease.
Peptic ulcers occur when the protective mucous lining in your stomach and duodenum has been eroded, allowing gastric acids and digestive enzymes to eat away at your stomach and duodenal walls. This eventually results in open sores that are continually irritated by the acid. If left untreated, they can begin to cause serious complications, such as internal bleeding. Over time, they can even wear a hole all the way through. This is a medical emergency.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Stomach ulcers are very common in Western countries. In the United States, there are about 4 million cases per year. Some estimates say that 1 in 10 people will have one at some point in their lives. That’s because many of the causes that contribute to stomach ulcers are common in Western life. Fortunately, these causes are usually easy to trace and to reverse, giving ulcers a chance to heal and your stomach lining a chance to repair.
The two most common causes are:
Less common causes of stomach ulcers include:
Advertisement
Some peptic ulcers don’t cause symptoms. These are called “silent ulcers." But the following symptoms are common with both duodenal and gastric ulcers:
The classic symptoms of peptic ulcers are stomach pain and indigestion. Ulcer pain feels like burning or gnawing inside your stomach, which is between your breastbone and your belly button. It may improve temporarily when you eat or drink or when you take an antacid, medication to reduce stomach acid. It may feel worse between meals and at night when stomach acid builds up without food to digest. It may also make you feel like you don’t want to eat.
Gastritis and gastric ulcers share many symptoms and often go hand in hand. Gastritis can be a precursor to stomach ulcers, caused by the same conditions that will eventually cause ulcers, including H. pylori infection and mucous erosion. You may also have both.
Both gastritis and stomach ulcers can cause stomach pain, as well as symptoms of indigestion. Usually, the pain from an ulcer will feel more localized — like it’s coming from one particular spot. But since some ulcers are “silent,” you might not feel it if you do have one.
If you have symptoms of either gastritis or stomach ulcer, you should seek medical care. Gastritis can lead to ulcers if it hasn’t already. It can also indicate an infection or other condition that needs to be treated. Medical testing can quickly determine the causes of your stomach pain.
Ulcer pain in your stomach area can feel very similar to heartburn. It’s often described as a burning kind of pain. Usually, ulcer pain will be localized at the site of the ulcer, which is in the stomach or small intestine. Heartburn covers a broader area and tends to be higher into the chest. However, you could have heartburn and ulcer pain at the same time.
Heartburn is usually caused by acid reflux, which is when acid from your stomach travels back up through your esophagus. So, heartburn may start as low as your stomach, but it will also travel upwards from there. If your pain is higher than your breast bone, that’s probably heartburn — but it doesn’t mean you don’t have an ulcer too. Acid reflux can also be a symptom of a stomach ulcer.
Advertisement
Stomach ulcers are irritated by stomach acid. Some people notice this irritation more after they eat, and some people notice it more on an empty stomach. There are also certain irritants that seem to make ulcer symptoms worse and make them more difficult to heal. Smoking and alcohol are the biggest ones.
An ulcer left untreated may cause serious complications, including:
Bleeding ulcers don’t always cause pain. Sometimes the first signs of a bleeding ulcer are signs of anemia. These include:
You might have a heavier bleed if you notice:
These symptoms require urgent medical attention.
Your healthcare provider will ask you about your symptoms and medical history. They will want to know if you frequently use NAIDs or have a history of H. pylori infection. If signs point to an ulcer, they will want to take a look inside your stomach and duodenum.
Endoscopy. An upper endoscopy exam is expedient because allows healthcare providers to see inside your digestive tract and also take a tissue sample to analyze in the lab. The test is done by passing a thin tube with a tiny camera attached down your throat and into your stomach and duodenum. You’ll have medication to numb your throat and help you relax during the test. Your healthcare provider may use the endoscope to take a tissue sample to test for signs of mucous damage, anemia, H. pylori infection or malignancy. If they take a sample, you won’t feel it.
Imaging tests. Imaging tests to look inside the stomach and small intestine include:
Tests for H. pylori. Your healthcare provider might want to test you separately for H. pylori infection. Tests may include:
Breath test. The H. pylori breath test is an accurate test for diagnosing an active H. pylori infection. For the test, you’ll drink a flavored solution containing an organic chemical compound called urea. If H. pylori bacteria are present in your digestive tract, they will break down the urea and convert it to carbon dioxide. The carbon dioxide will come out in your breath. When you breathe into a bag, healthcare providers will be able to measure it.
Ulcers can heal if they are given a rest from the factors that created them. Healthcare providers treat uncomplicated ulcers with a combination of medicines to reduce stomach acid, coat and protect the ulcer during healing and kill any bacterial infection that may be involved. Medicines may include:
While most ulcers are successfully treated with medication, some complicated ulcers may require surgery. Ulcers that are bleeding, or that have perforated your stomach or intestinal wall, will need to be surgically repaired. An ulcer that is malignant, or obstructing a passageway, will need to be surgically removed. In severe cases, an ulcer that keeps coming back may be treated by surgery to cut off some of the nerve supply to the stomach that produces stomach acid.
If you take all medicines as prescribed and avoid irritating the ulcer with NSAIDs, alcohol or smoking, your ulcer should heal well within a few weeks. Surgical cases may take a few weeks more. Your healthcare provider will follow up with you at the end of your course of medication to make sure the ulcer has healed and any infection has cleared. They will probably take follow-up tests, including an upper endoscopy to look at the site of the ulcer and tests for H. pylori, if you had it, to make sure the infection is gone.
It’s a good idea to be conscious of your diet and avoid things that might aggravate your ulcer and prolong the healing process. Balance overly acidic foods, including grains, dairy and meat products, with alkaline foods such as fruits and vegetables. Avoid alcohol and caffeine while healing.
Some ulcers follow a chronic pattern of healing temporarily on their own and then returning. This might happen if the factors contributing to your ulcer, such as NSAID use, smoking and alcohol, are temporarily reduced and then resumed. You won’t completely heal your ulcer until you eliminate the cause, whether that is chronic NSAID use, H. pylori infection or an overactive stomach. Even after successful treatment, you can get another ulcer.
Always seek medical care for a stomach ulcer. While you may be able to manage symptoms temporarily with over-the-counter medications, these won’t heal the ulcer. You need to identify and treat the underlying cause. An untreated ulcer can lead to serious complications, even if your symptoms are mild. The major cause of stomach ulcers, H. pylori infection, can also lead to other complications.
Seek emergency care if you have:
A note from Cleveland Clinic
Stomach ulcers are common and treatable, but they should be taken seriously. Even when they don’t cause symptoms, they aren’t a good sign. A stomach ulcer means that your natural stomach acid is overwhelming your protective stomach lining. That’s a situation that can only get worse if it isn’t managed. Lifestyle changes may help, but you’ll still need to treat the underlying cause. It’s probably either NSAID use or a common bacterial infection. Your healthcare provider can help prescribe the right medicines for your condition.
Last reviewed on 02/01/2022.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy