“Lymphoma” is a term for a group of blood cancers in your lymphatic system. There are two types of lymphoma — Hodgkin lymphoma and non-Hodgkin lymphoma. Healthcare providers can successfully treat and often cure it.
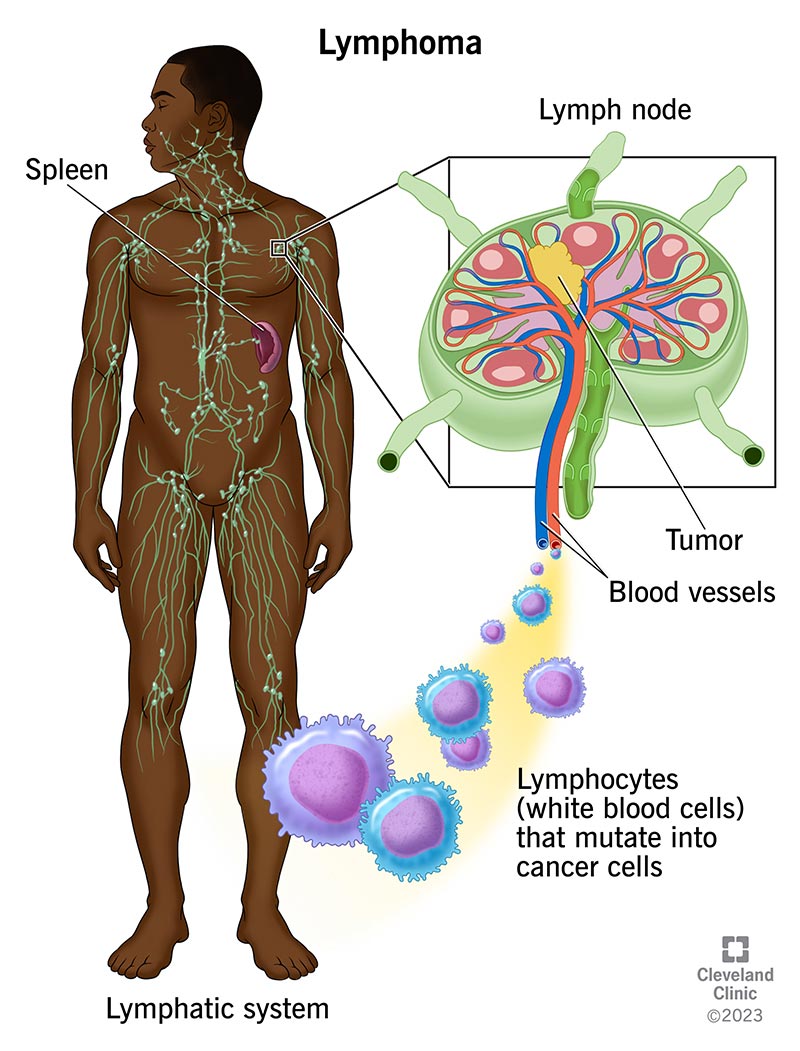
“Lymphoma” is the general term for cancer in your lymphatic system — the network of tissues, vessels and organs that help your body fight infection. It’s considered a blood cancer because the condition starts in white blood cells (lymphocytes) in your lymphatic system.
There are two main lymphoma categories — Hodgkin lymphoma and non-Hodgkin lymphoma — and more than 70 lymphoma subtypes. Lymphomas can be aggressive (fast-growing) or indolent (slow-growing). Often, treatment can put lymphoma into remission or cure it. Children, teenagers and adults may develop lymphoma. This article focuses on lymphomas that affect adults.
No, lymphoma isn’t common. The American Cancer Society estimates 89,000 people in the U.S. will be diagnosed with lymphoma in 2023. For comparison, 236,740 people in the U.S. will receive a lung cancer diagnosis in 2023.
Non-Hodgkin typically affects ages 60 to 80. It’s more common in men and people assigned male at birth (AMAB) than in women and people assigned female at birth (AFAB).
Hodgkin lymphoma may affect people between the ages of 20 to 39 and at or over age 65. Men and people AMAB are slightly more likely to develop Hodgkin lymphoma than women and people AFAB.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Many lymphoma symptoms are like symptoms of other, less serious diseases. Having these symptoms doesn’t mean that you have lymphoma. But you should consider talking to a healthcare provider whenever you have changes in your body that don’t go away within a few weeks.
Symptoms common to Hodgkin lymphoma and non-Hodgkin lymphoma can include:
Lymphoma happens when the white blood cells in your lymphatic system change (mutate) into rapidly growing cancer cells that don’t die. Like most cancers, the majority of the genetic mutations that cause lymphoma happen spontaneously, without an identifiable cause. But research suggests the following conditions or issues may increase your risk of developing lymphoma:
Advertisement
Healthcare providers diagnose lymphoma by doing physical examinations to evaluate potential lymphoma symptoms and biopsies to obtain tissue for examination by a medical pathologist. If laboratory tests show signs of lymphoma, providers may do certain blood and imaging tests to learn more about your condition and to plan treatment.
Blood tests
Imaging tests
If you have non-Hodgkin lymphoma, your provider may order laboratory tests to identify genes, proteins and other substances that are unique to specific non-Hodgkin lymphomas.
Treatments vary based on lymphoma type. For example, if you have a slow-growing lymphoma, your healthcare provider may recommend active surveillance (watchful waiting) before starting treatment. In active surveillance, providers carefully monitor your overall health and signs of lymphoma.
Common lymphoma treatments include:
Your provider may recommend palliative care as part of your treatment plan. Palliative care focuses on helping you manage symptoms and treatment side effects. It also offers support. Palliative care treatment may include medication, activities to help manage stress, and emotional and spiritual support.
Lymphoma treatments may have different side effects because people often have different reactions to the same treatment. Ask your healthcare provider about treatment side effects and what you can do to manage them.
Advertisement
Researchers continue to identify lymphoma risk factors. There’s reason to believe certain viruses and family medical history increase the risk of developing lymphoma. Talk to your healthcare provider if you think your medical history or family medical history might increase your risk of developing lymphoma.
Your prognosis is what you can expect after completing treatment. Your specific prognosis depends on your situation, such as the type of lymphoma you have, your age and your overall health. That said, treatment often puts lymphoma into remission or cures the condition. Remission means you don’t have lymphoma symptoms and tests don’t find signs of lymphoma.
Lymphoma in remission can come back (recur). If you have lymphoma in remission, you’ll have regular follow-up appointments with your healthcare provider. They may do tests to check for signs of lymphoma. Symptoms are changes that you can feel in your body and describe to others. Signs are changes in something measured, like your temperature or blood tests to check white blood cell counts.
Overall, survival rate data show 89% of people with Hodgkin lymphoma and 74% of people with non-Hodgkin lymphoma were alive five years after diagnosis.
Survival rates are estimates based on the experiences of groups of people with the same disease. Survival rate estimates can’t predict how long a person may live with lymphoma. If you have questions about lymphoma survival rates, ask your healthcare provider to explain what you can expect.
If you have lymphoma, you might benefit by creating a plan for living with lymphoma. This plan could see you through initial treatment and any follow-up treatment. Here are some things to consider as you develop your plan:
Contact your healthcare provider any time you think your lymphoma symptoms are getting worse or you need help managing your treatment side effects.
Many cancer treatments affect your immune system. That means your cancer treatment might increase your risk of developing infections. Symptoms that might require an emergency room visit are:
Cancer is a journey, and your questions will change throughout your journey. If you’re just learning you have lymphoma, here are some basic questions you might want to ask:
That depends on the type of lymphoma. For example, non-Hodgkin lymphoma may make your body more vulnerable to life-threatening infections, other kinds of cancer or heart disease. Data show about 3 in 100,000 people worldwide die of some type of non-Hodgkin lymphoma.
Blood tests may detect issues like having a high white blood cell count that may be a sign of lymphoma, leukemia or other blood cancers. But they don’t detect lymphoma. Healthcare providers diagnose lymphoma based on biopsy and imaging tests results.
Lymphoma can start almost anywhere you have lymphocytes. These are infection-fighting white blood cells that are found throughout your lymphatic system. You have lymphocytes in your lymph nodes, spleen, bone marrow and other areas of your body. The most common early symptom is swollen lymph nodes in your neck, upper chest, armpit, belly or groin.
You can have lymphoma for years without noticing changes in your body. Sometimes, people learn they have the condition of lymphoma because routine imaging tests detect signs of lymphoma.
A note from Cleveland Clinic
Lymphoma is a serious illness. Fortunately, lymphoma treatments continue to improve, helping people live longer. Each year, survival rates improve. And researchers are learning more about lymphoma risk factors. Talk to your healthcare provider if you think you might be at risk for lymphoma. If you are, they can help you understand what you can do to protect your health.
Last reviewed on 06/09/2023.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy