Menopause is a point in time when a person has gone 12 consecutive months without a menstrual period. Menopause is a natural part of aging and marks the end of your reproductive years. On average, menopause happens at age 51.
Menopause is a point in time when you’ve gone 12 consecutive months without a menstrual cycle. The time leading up to menopause is called perimenopause. This is when a lot of women or people assigned female at birth (AFAB) start to transition to menopause. They may notice changes in their menstrual cycles or have symptoms like hot flashes.
Natural menopause is the permanent ending of menstruation that doesn’t happen because of any type of medical treatment. The process is gradual and happens in three stages:
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The average age of menopause in the United States is approximately 51 years old. However, the transition to menopause usually begins in your mid-40s.
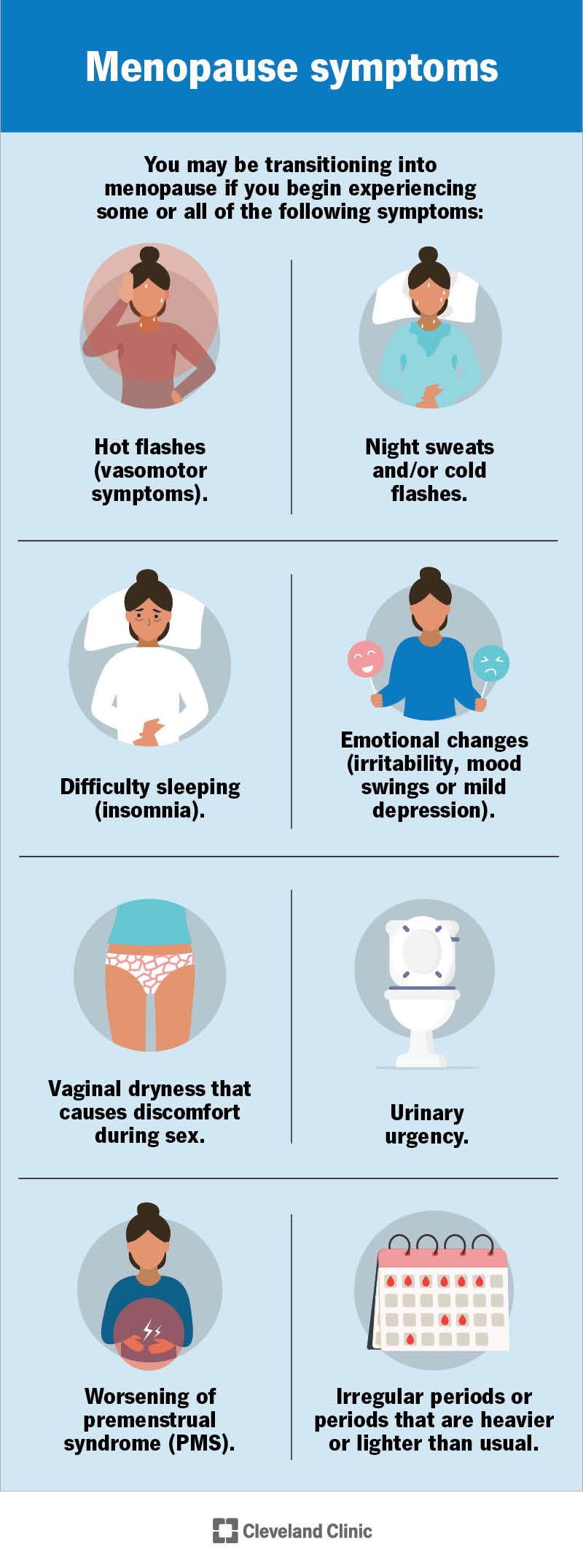
You may be transitioning into menopause if you begin experiencing some or all of the following symptoms:
Some people might also experience:
Changes in your hormone levels cause these symptoms. Some people may have intense symptoms of menopause, while others have mild symptoms. Not everyone will have the same symptoms as they transition to menopause.
Contact a healthcare provider if you’re unsure if your symptoms are related to menopause or another health condition.
You can have symptoms of menopause for up to 10 years. However, most people experience symptoms of menopause for less than five years.
Advertisement
Hot flashes are one of the most frequent symptoms of menopause. It’s a brief sensation of heat. Aside from the heat, hot flashes can also come with:
The intensity, frequency and duration of hot flashes differ for each individual. Typically, hot flashes are less severe as time goes on.
When menopause happens on its own (natural menopause), it’s a normal part of aging. Menopause is defined as a complete year without menstrual bleeding, in the absence of any surgery or medical condition that may cause bleeding to stop such as hormonal birth control, radiation therapy or surgical removal of your ovaries.
As you age, your reproductive cycle begins to slow down and prepares to stop. This cycle has been continuously functioning since puberty. As menopause nears, your ovaries make less of a hormone called estrogen. When this decrease occurs, your menstrual cycle (period) starts to change. It can become irregular and then stop.
Physical changes can also happen as your body adapts to different levels of hormones. The symptoms you experience during each stage of menopause (perimenopause, menopause and postmenopause) are all part of your body’s adjustment to these changes.
Advertisement
The traditional changes we think of as “menopause” happen when your ovaries no longer produce high levels of hormones. Your ovaries are the reproductive glands that store and release eggs. They also produce the hormones estrogen and progesterone. Together, estrogen and progesterone control menstruation. Estrogen also influences how your body uses calcium and maintains cholesterol levels in your blood.
As menopause nears, your ovaries no longer release eggs, and you’ll have your last menstrual cycle.
You’ll know you’ve reached menopause when you’ve gone 12 consecutive months without a menstrual period. Contact your healthcare provider if you have any type of vaginal bleeding after menopause. Vaginal bleeding after menopause could be a sign of a more serious health issue.
There are several ways your healthcare provider can diagnose menopause. The first is discussing your menstrual cycle over the last year. Menopause is unique in that your provider diagnoses it after it occurs. If you’ve gone a full year (12 straight months) without a period, you’ve entered menopause and may be postmenopausal.
Menopause is a natural process that your body goes through. In some cases, you may not need any treatment for menopause. When discussing treatment for menopause with your provider, it’s about treating the symptoms of menopause that disrupt your life. There are many different types of treatments for the symptoms of menopause. The main types of treatment for menopause are:
It’s important to talk to your healthcare provider while you’re going through menopause to craft a treatment plan that works for you. Every person is different and has unique needs.
During menopause, your body goes through major hormonal changes — decreasing the amount of hormones it makes. Your ovaries produce estrogen and progesterone. When your ovaries no longer make enough estrogen and progesterone, hormone therapy can make up for lost hormones. Hormone therapy boosts your hormone levels and can help symptoms like hot flashes and vaginal dryness. It can also help prevent osteoporosis.
There are two main types of hormone therapy:
The health risks of hormone therapy include:
These risks are lower if you start hormone therapy within 10 years of menopause. After that point, your risk for cardiovascular diseases is higher.
A correlation exists between severe hot flashes and night sweats and your risk for cardiovascular disease. Healthcare providers may suggest starting hormone therapy if you have these severe symptoms since it’s an indicator for future cardiovascular risk.
Going on hormone therapy is an individualized decision. Discuss all past medical conditions and your family history with your healthcare provider to understand the risks versus benefits of hormone therapy.
Though hormone therapy is a very effective method for relieving menopause symptoms, it’s not the perfect treatment for everyone. Nonhormonal treatments include changes to your diet and lifestyle. These treatments are often good options for people who have other medical conditions or have recently been treated for breast cancer. The main nonhormonal treatments that your provider may recommend include:
Sometimes changing your diet can help relieve menopause symptoms. Limiting the amount of caffeine you consume every day and cutting back on spicy foods can make your hot flashes less severe. You can also add foods that contain plant estrogen into your diet. Plant estrogen (isoflavones) isn’t a replacement for the estrogen your body makes before menopause. Foods to try include:
Certain things in your daily life could be triggers for hot flashes. To help relieve your symptoms, try and identify these triggers and work around them. This could include keeping your bedroom cool at night, wearing layers of clothing or quitting smoking. Weight loss can also help with hot flashes.
Working out can be difficult if you’re dealing with hot flashes, but exercising can help relieve several other symptoms of menopause. Exercise can help you sleep through the night and is recommended if you have insomnia. Calm, tranquil types of exercise like yoga can also help with your mood and relieve any fears or anxiety you may be feeling.
Talking to other people who are also going through menopause can be a great relief for many. Joining a support group can not only give you an outlet for the many emotions running through your head, but also help you answer questions you may not even know you have.
Prescription medications such as estrogen therapy (estrogen in a cream, gel or pill), birth control pills and antidepressants (SSRIs and SNRIs) can help manage symptoms of menopause like mood swings and hot flashes. Prescription vaginal creams can help relieve vaginal dryness. A seizure medication called gabapentin has been shown to relieve hot flashes. Speak with your healthcare provider to see if nonhormonal medications could work for managing your symptoms.
The possibility of pregnancy disappears once you’re postmenopausal. However, you can get pregnant during the menopause transition (perimenopause). If you don’t want to become pregnant, you should continue to use some form of birth control until you’re sure you’ve gone through menopause. Ask your healthcare provider before you stop using contraception.
There are several conditions that you could be at a higher risk of after menopause. Your risk for any condition depends on many things like your family history, your health before menopause and lifestyle factors. Two conditions that affect your health after menopause are osteoporosis and coronary artery disease.
Osteoporosis, a “brittle-bone” disease, occurs when the insides of bones become less dense, making them more fragile and likely to fracture. Estrogen plays an important role in preserving bone mass. Estrogen signals cells in the bones to stop breaking down.
People lose an average of 25% of their bone mass from the time of menopause to age 60. This is largely because of the loss of estrogen. Over time, this loss of bone can lead to bone fractures. Your healthcare provider may want to test the strength of your bones over time. Bone mineral density testing, also called bone densitometry, is a quick way to see how much calcium you have in certain parts of your bones. The test is used to detect osteoporosis and osteopenia. Osteopenia is a disease where bone density is decreased and this can be a precursor to later osteoporosis.
If you have osteoporosis or osteopenia, your treatment options could include estrogen therapy.
Coronary artery disease is the narrowing or blockage of arteries that supply your heart muscle with blood. This happens when fatty plaque builds up in the artery walls (known as atherosclerosis). This buildup is associated with high levels of cholesterol in your blood. After menopause, your risk for coronary artery disease increases because of several things, including:
The benefits and risks of hormone therapy vary depending on your age and health history. In general, younger people in their 50s tend to get more benefits from hormone therapy compared to those who are postmenopausal in their 60s. People who undergo premature menopause often receive hormone therapy until age 50 to make up for the extra years of estrogen loss.
Some people may experience trouble sleeping through the night and insomnia during menopause. This can be a normal side effect of menopause itself, or it could be due to another symptom of menopause. Hot flashes are a common culprit of sleepless nights during menopause.
After menopause, your body has less estrogen. This major change in your hormonal balance can affect your sex life. Many people experiencing menopause may notice that they’re not as easily aroused as before. Sometimes, people also may be less sensitive to touch and other physical contact than before menopause.
These feelings, coupled with the other emotional changes you may be experiencing, can all lead to a decreased interest in sex. Keep in mind that your body is going through a lot of change during menopause. Some of the other factors that can play a role in a decreased sex drive can include:
All of these factors can disrupt your life and even cause tension in your relationship(s). In addition to these changes, the lower levels of estrogen in your body can cause a decrease in the blood supply to your vagina. This can cause dryness. When you don’t have the right amount of lubrication in your vagina, it can lead to painful intercourse.
Don’t be afraid to talk to your healthcare provider about any decreases you’re experiencing in your sex drive. Your provider will discuss options to help you feel better. For example, you can treat vaginal dryness with over-the-counter (OTC), water-soluble or silicone lubricants. Your healthcare provider can also prescribe estrogen or non-estrogen hormones to treat the vaginal tissue. They can prescribe this in a low-dose cream, pill or vaginal ring.
Not all people experience a decreased sexual desire. In some cases, it’s just the opposite. This could be because there’s no longer any fear of getting pregnant. For many, this allows them to enjoy sex without worrying about family planning.
However, it’s still important to use protection (condoms) during sex if you’re not in a monogamous relationship. You still need to protect yourself from sexually transmitted infections (STIs). You can get an STI at any time in your life, even after menopause.
No, you can’t get pregnant after menopause because ovulation is no longer occurring.
It may. Hormone changes can impact your weight. For example, you may start to lose muscle as you get older, which can affect how your body gains weight.
Yes. Your teeth and gums are susceptible to the hormonal changes that occur during menopause. This can lead to noticeable symptoms like a dry mouth or sensitive teeth and gums. This could increase your risk of developing cavities or gingivitis.
Yes. One of the symptoms of the transition to menopause is dry eyes.
Yes, facial hair growth can be a change related to menopause. This is because testosterone is relatively higher than estrogen. If facial hair becomes a problem for you, waxing or using other hair removers may be options.
Unfortunately, concentration and minor memory problems can be a normal part of menopause. Though this doesn’t happen to everyone, it can happen. If you’re having memory problems during menopause, call your healthcare provider. Several activities have been shown to stimulate the brain and help rejuvenate your memory. These activities can include:
Menopause, when it occurs between the ages of 45 and 55, is considered “natural” and is a normal part of aging. Menopause that occurs before the age of 45 is called early menopause. Menopause that occurs at 40 or younger is considered premature menopause. When there’s no medical or surgical cause for premature menopause, it’s called primary ovarian insufficiency.
Yes, several factors related to menopause can lead to depression. Your body goes through a lot of changes during menopause. There are extreme shifts in your hormone levels, you may not sleep well because of hot flashes and you may experience mood swings. Anxiety and fear could also be at play during this time.
If you experience any of the symptoms of depression, talk to your healthcare provider. During your conversation, your provider will tell you about different types of treatment and check to make sure there isn’t another medical condition causing your depression.
Menopause can cause a variety of emotional changes, including:
All of these emotional changes can happen outside of menopause, too. You’ve probably experienced some of them throughout your life.
Your healthcare provider may be able to prescribe a medication to help you (hormone therapy or an antidepressant). It may also help to just know that there’s a name for the feelings you’re experiencing. Support groups and counseling are useful tools when dealing with emotional changes during menopause.
Unfortunately, bladder control issues (also called urinary incontinence) are common for people going through menopause. There are several reasons why this happens, including:
It depends on if your surgeon also removed your ovaries during the hysterectomy. If you kept your ovaries, you may not have symptoms of menopause right away. If your surgeon also removes your ovaries, you’ll have symptoms of menopause immediately.
Yes, you can still have an orgasm after menopause. An orgasm may feel hard to achieve once you’ve reached menopause, but there’s no physical reason to prevent you from having an orgasm.
Andropause, or male menopause, is a term that describes decreasing testosterone levels in men or people assigned male at birth (AMAB). Testosterone production in men declines about 1% per year — much more gradually than estrogen production in women. Healthcare providers often debate calling this slow decline in testosterone “menopause” since it’s not as drastic of a hormone shift and doesn’t carry the same intensity of side effects as menopause in women. Some men won’t even notice the change because it happens over many years or decades. Other names for the male version of menopause are age-related low testosterone, male hypogonadism or androgen deficiency.
A note from Cleveland Clinic
Menopause is a natural and normal part of the aging process. Once you’re in menopause, you’ve gone 12 months without a menstrual period. It’s common to experience symptoms like vaginal dryness and hot flashes. Be open with your healthcare provider about the symptoms you’re experiencing and how they impact your quality of life. They can recommend treatments to manage your symptoms and make you more comfortable.
Last reviewed on 10/05/2021.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy