Type 2 diabetes happens when your body can’t use insulin properly. Without treatment, Type 2 diabetes can cause various health problems, like heart disease, kidney disease and stroke. You can manage this disease by making lifestyle changes, taking medications and seeing your healthcare provider for regular check-ins.
Type 2 diabetes (T2D) is a chronic condition that happens when you have persistently high blood sugar levels (hyperglycemia).
Healthy blood sugar (glucose) levels are 70 to 99 milligrams per deciliter (mg/dL). If you have undiagnosed Type 2 diabetes, your levels are typically 126 mg/dL or higher.
T2D happens because your pancreas doesn’t make enough insulin (a hormone), your body doesn’t use insulin properly, or both. This is different from Type 1 diabetes, which happens when an autoimmune attack on your pancreas results in a total lack of insulin production.
Type 2 diabetes is very common. More than 37 million people in the U.S. have diabetes (about 1 in 10 people), and about 90% to 95% of them have T2D.
Researchers estimate that T2D affects about 6.3% of the world’s population. T2D most commonly affects adults over 45, but people younger than 45 can have it as well, including children.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
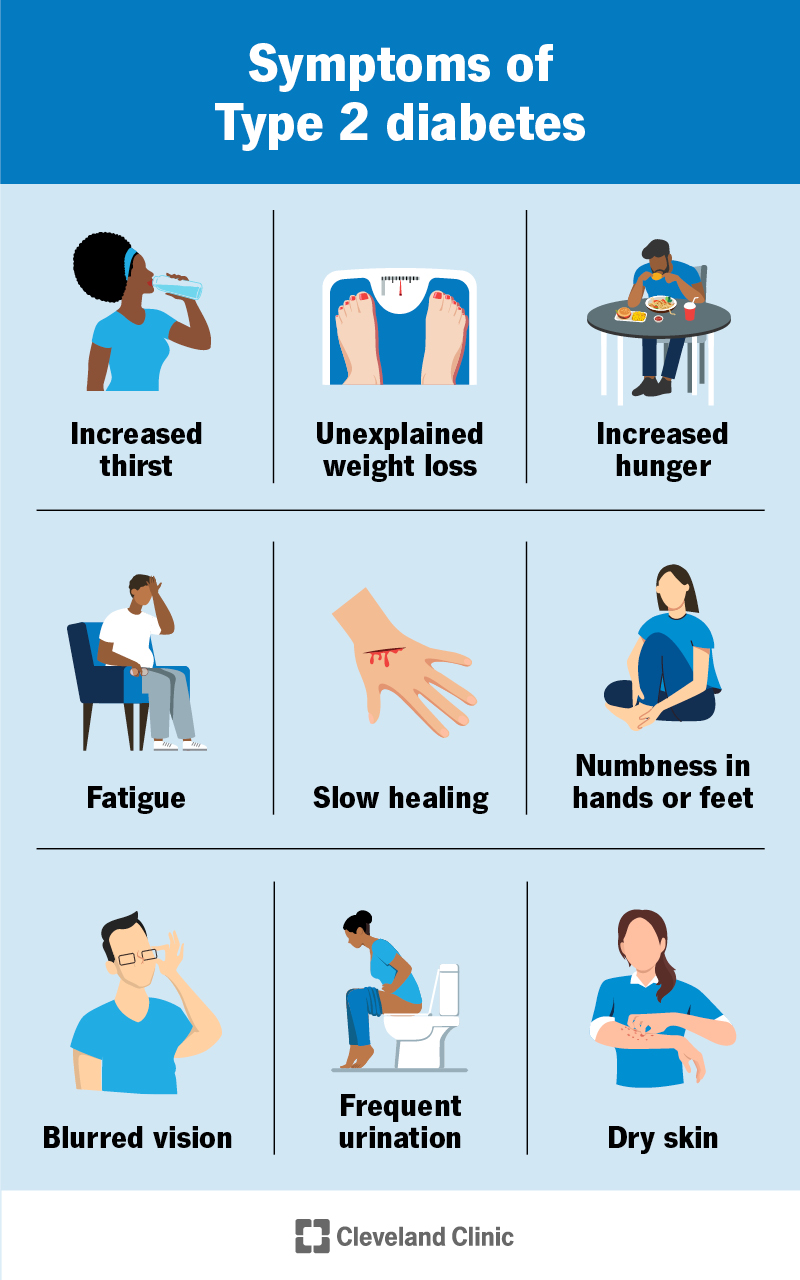
Symptoms of Type 2 diabetes tend to develop slowly over time. They can include:
People assigned female at birth (AFAB) may experience frequent vaginal yeast infections and/or urinary tract infections (UTIs).
If you have these symptoms, it’s important to see your healthcare provider. Simple blood tests can diagnose T2D.
The main cause of Type 2 diabetes is insulin resistance.
Insulin resistance happens when cells in your muscles, fat and liver don’t respond as they should to insulin. Insulin is a hormone your pancreas makes that’s essential for life and regulating blood sugar levels.
If your body isn’t responding to insulin properly, your pancreas has to make more insulin to try to overcome your increasing blood glucose levels (hyperinsulinemia). If your cells become too resistant to insulin and your pancreas can’t make enough insulin to overcome it, it leads to Type 2 diabetes.
Several factors can contribute to insulin resistance, including:
The cause of T2D is complex, but researchers know that genetics play a strong role. Your lifetime risk of developing T2D is 40% if you have one biological parent with T2D and 70% if both of your biological parents have it.
Researchers have identified at least 150 DNA variations linked to the risk of developing T2D — some increase your risk and others decrease it. Some of these variations may directly play a role in insulin resistance and insulin production. Others may increase your risk of T2D by increasing your tendency to have overweight or obesity.
These genetic variations likely act together with health and lifestyle factors to influence your overall risk of T2D.
You’re more likely to develop Type 2 diabetes if you:
As T2D symptoms typically come on slowly, it’s important to see your primary care provider regularly if you’re at risk for the condition. This way, they can do screenings, like a basic metabolic panel (BMP), to check on your blood sugar levels. It’s better to catch T2D earlier rather than later.
Advertisement
The following blood tests help your healthcare provider diagnose Type 2 diabetes:
In some cases, your provider may order an autoantibody blood test to see if you have Type 1 Diabetes instead of T2D.
Unlike many health conditions, you mainly manage T2D on your own with medical guidance and support from your healthcare team. This could include your:
Your team should also include family members and other important people in your life. Managing T2D can be challenging — you have to make several decisions every day for it. But everything you do to improve your health is worth it.
The core features of Type 2 diabetes management include:
Regular activity is important for everyone. It’s even more important if you have diabetes. Exercise is good for your health because it:
Talk to your provider before starting any exercise program. You may need to take special steps before, during and after physical activity, especially if you take insulin. The general goal is to get at least 150 minutes per week of moderate-intensity physical activity.
Ask your healthcare provider or registered dietitian to recommend a meal plan that’s right for you. What you eat, how much you eat, and when you eat are all important in keeping your blood sugar levels in the range that your healthcare team recommends.
The key to eating with Type 2 diabetes is to eat a variety of nutritious foods from all food groups, in the amounts your meal plan outlines. In general, these types of foods can help support healthy blood sugar levels:
Monitoring your blood sugar is essential to finding out how well your current treatment plan is working. It gives you information on how to manage diabetes on a daily — and sometimes even hourly — basis. The results of blood sugar monitoring can help you make decisions about food, physical activity and dosing insulin.
Several things can affect your blood sugar. You can learn to predict some of these impacts with time and practice, while others are very difficult or impossible to predict. That’s why it’s important to check your blood sugar regularly if your healthcare provider recommends doing so.
There are two main ways you can monitor your blood sugar at home if you have diabetes:
You may choose either or both methods for a variety of reasons, such as:
Your healthcare provider may recommend taking medication, in addition to lifestyle changes, to manage Type 2 diabetes. These include:
Advertisement
Type 2 diabetes is a chronic (long-term) disease, which means you must manage it for the rest of your life. There’s no cure for T2D. But you can manage it — with lifestyle changes, medication and blood sugar monitoring — in a way that keeps your blood sugar levels in a healthy range. If you stop managing it or undermanage it, your blood sugar levels will go back up.
Certain strategies can help lower your risk of developing Type 2 diabetes or delay its onset, including:
Unfortunately, some people have such strong genetic risk factors that even lifestyle changes aren’t enough to prevent developing T2D.
If you have Type 2 diabetes, your outlook depends on several factors, like:
Untreated or undermanaged T2D can lead to a range of health conditions.
As your blood touches virtually every part of your body, having undermanaged Type 2 diabetes that results in continuous high blood sugar over a long period of time can damage several areas of your body.
Potential complications of Type 2 diabetes include:
Cardiovascular disease, including:
Eye conditions, including:
Additional complications include:
Hyperosmolar hyperglycemic state (HHS) is a life-threatening complication of Type 2 diabetes. HHS happens when your blood sugar levels are too high for a long period, leading to severe dehydration and confusion.
Symptoms of HHS usually come on slowly and can take days or weeks to develop. Symptoms include:
HHS is life-threatening and requires immediate medical treatment. If you experience these symptoms, call 911 or your local emergency services number.
Type 2 diabetes is a complex condition that requires daily management, effort and planning. Some tips that can help you manage T2D include:
You’ll need to have regular appointments with your healthcare team to be sure you’re on track with your T2D management plan. As your body, life and routines change, your management will need to, as well. Your healthcare team can provide new strategies that are unique to your needs.
If you develop symptoms of any diabetes complications, be sure to see your provider as soon as possible.
A note from Cleveland Clinic
Type 2 diabetes involves constant day-to-day care and management. While it’ll likely be very overwhelming at first, over time you’ll get a better grasp on how to manage the condition and how to be in tune with your body.
Be sure to see your healthcare team regularly. Managing Type 2 diabetes involves a team effort — you’ll want both medical professionals and friends and family on your side. Don’t hesitate to reach out to them if you need help.
Last reviewed on 11/08/2023.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy