Patellofemoral pain syndrome (PFPS) is knee pain under or around your patella (kneecap). Experts aren’t certain what causes it, but you can usually treat it with the RICE method, physical therapy and by slowly ramping up your activity level.
Patellofemoral pain syndrome (PFPS) is knee pain under or around your kneecap (patella). Healthcare providers also sometimes call PFPS runner’s knee.
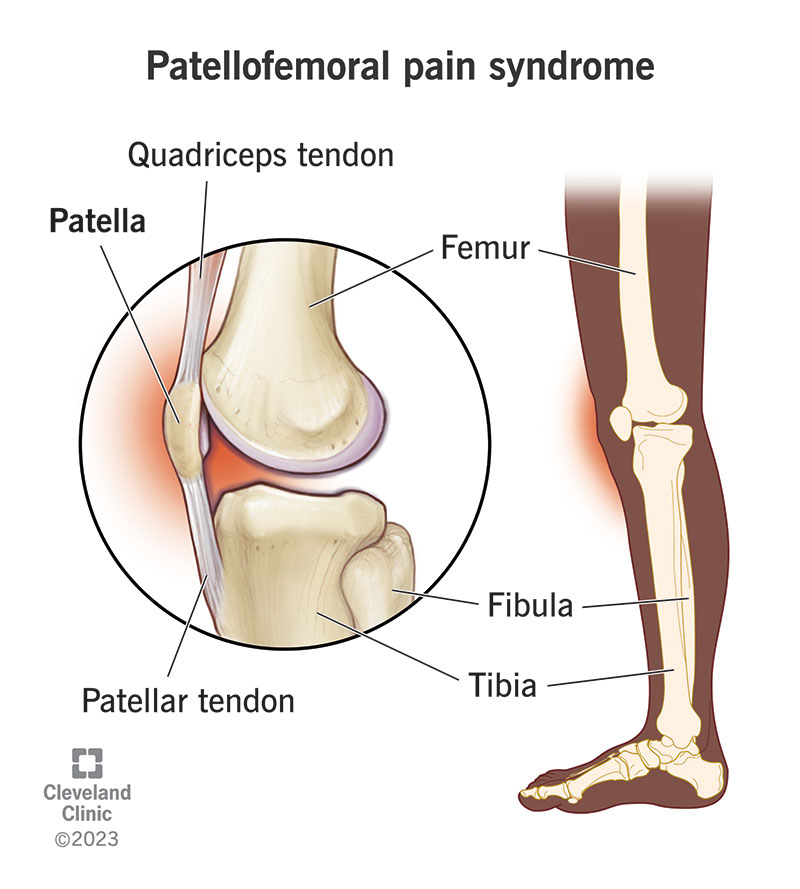
Your patella is the bone at the front of your knee joint. It helps your quadriceps muscle move your leg, protects your knee, and supports lots of important muscles, tendons and ligaments.
“Patellofemoral” is the medical term for the connection between your patella and your thigh bone (femur). Usually, your patella fits into a groove in your femur and slides smoothly along that space when you move your knee. If you have PFPS, something may affect how your patella moves and make it painful.
People usually develop PFPS over time. It can affect one or both of your knees at once. Visit a healthcare provider if you’re experiencing knee pain that doesn’t get better in a few weeks.
PFPS is very common. Experts estimate that around one-third of people who visit healthcare providers with knee pain have PFPS.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Pain in the front of your knee is the most common PFPS symptom. You might also hear or feel cracking or popping in your knees.
Patellofemoral pain syndrome usually develops over time. The pain typically gets worse when you:
PFPS usually feels like a dull ache at the front of your knee or on the sides near your patella. It might feel sharp or stabbing during activities or while you’re running, jumping, squatting or on stairs.
Experts aren’t sure exactly what causes PFPS. Some factors or issues that may cause it include:
Anyone can develop PFPS, especially if you’ve recently changed your activity level. Some groups of people are more likely to experience it, including:
Advertisement
PFPS usually gets worse over time if it’s not diagnosed and treated. On top of increasing pain, untreated PFPS may increase your risk of injuries. The pain can make you hold and carry your body differently (your posture), even if you’re not thinking about it. This can put extra stress on joints like your hips and ankles, or muscles in your legs, abdomen or back.
A healthcare provider will diagnose PFPS with a physical exam. They’ll examine your knees and ask about your symptoms. Tell your provider when you first noticed pain and other symptoms, and if any activities make them worse.
Your provider might ask you to move or use your knees. They may bend your knee, ask you to hold your leg straight out in front of you or squat. Tell your provider if any of these movements hurt or make the pain worse.
You might need a knee X-ray or magnetic resonance imaging (MRI) to take pictures of your knee joint and tissue that supports it.
Advertisement
Your provider will suggest PFPS treatments that relieve your pain and help you move comfortably, including:
You can usually treat PFPS at home with the RICE method:
A physical therapist will show you stretches and exercises that strengthen the muscles around your knees. Increasing your quad muscle strength and flexibility will support your knee better and help your patella move as it should.
Your healthcare provider might suggest medications to relieve PFPS. Most people can take over-the-counter NSAIDs (ibuprofen, aspirin and naproxen) or acetaminophen (Tylenol®). Don’t take these medications for more than 10 days in a row without talking to your provider.
You might need to wear a knee brace or special shoe inserts (orthotics) to stabilize your knee, ankle or lower leg.
Knee braces stabilize and support your knee joint. A knee brace can relieve pain when you’re physically active, especially early on when the pain is more intense. Talk to your provider about which type of brace will work best for you.
Orthotics are shoe inserts that you can buy over-the-counter or have custom-made. Your provider will tell you which kind you’ll need and how often to wear them.
It’s very rare to need surgery to treat PFPS. Your provider will probably only suggest knee surgery if you’re experiencing severe pain and other treatments haven’t helped.
If you do need surgery, your surgeon will likely perform a knee arthroscopy. They’ll make a few small incisions (cuts) in the skin around your knee, and then insert a special tool called an arthroscope into your knee joint. The arthroscope includes a camera and a light that lets your surgeon see and repair damage inside your knee.
You might be able to prevent PFPS, depending on what your provider thinks might have caused it. For example, you can slowly ramp up your activity level — especially if you’re starting a new sport or workout regimen. But you can’t prevent PFPS if your patella doesn’t naturally fit into its groove in your femur.
The best way to prevent PFPS (and any other type of knee pain) is to stay safe when you’re physically active. During sports or other physical activities:
Most people need a month or two to recover from patellofemoral pain syndrome. Your provider or physical therapist will give you a timeline based on your unique needs, strength and activity level.
You should expect to change or take a break from your usual activities while you’re managing PFPS. Most people can return to their usual sports or activities once they’re no longer feeling pain or other symptoms.
Visit a healthcare provider if you’re having knee pain that doesn’t get better on its own after a few weeks of rest and at-home treatments. Talk to your provider or physical therapist if you’ve started treatment for PFPS and your pain comes back or gets worse, especially if certain exercises or positions hurt.
Patellofemoral pain syndrome (PFPS) is a long way to say that your knee hurts when you’re working out or taking the stairs. But PFPS is usually straightforward to manage. Your healthcare provider or physical therapist will help you find ways to strengthen your muscles, increase your flexibility and manage the pain. Once you’re feeling strong and more stable on your knee, you should be able to resume all of your usual activities and sports.
Last reviewed on 12/19/2023.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy