Bradycardia is a condition where your heart beats more slowly than expected, under 60 beats per minute. For many people, it doesn’t cause symptoms and isn’t a problem, especially when it happens because you’re in very good physical shape. When it happens with symptoms, it’s usually a treatable condition with a positive outlook.
Bradycardia is a condition where your heart beats fewer than 60 times per minute, which is unusually slow. This condition may be dangerous if it keeps your heart from pumping enough blood to meet your body's needs. However, bradycardia can also happen without causing any harmful effects, especially in very physically active people.
Bradycardia and tachycardia are opposite conditions.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Bradycardia can happen to people of any age and background but is more common in adults over 65. It's less common in younger adults and children because your heart rate naturally slows down as you get older. The exception is when it happens because of certain conditions you're born with (genetic or otherwise).
It is also more common in people with certain conditions, some of which you can inherit from your parents, or if you take certain types of medication. It can also happen because of injuries to your chest or because of nutrition problems and eating disorders.
Bradycardia is a common condition among people in certain age groups and with certain circumstances. It’s most common in the following:
Advertisement
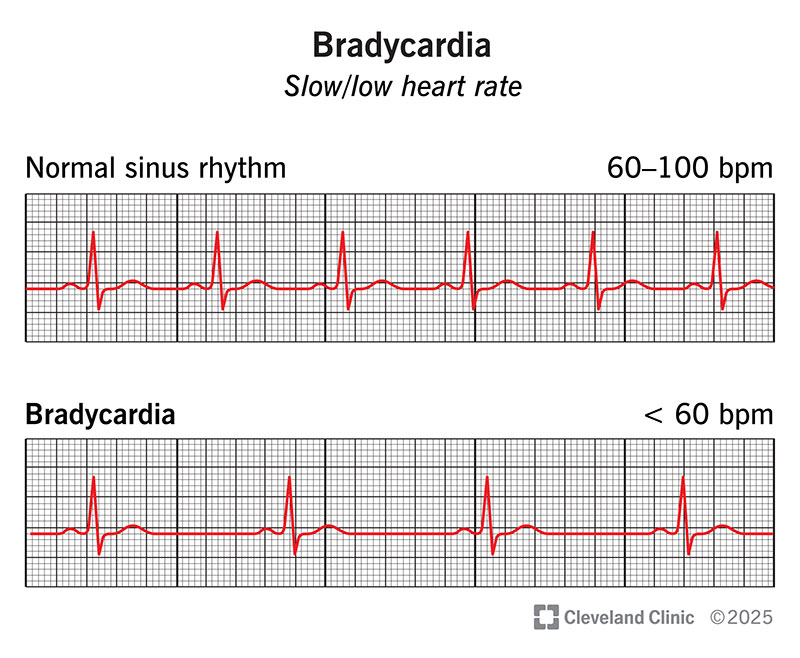
Bradycardia is an arrhythmia (abnormal heart rhythm) because it is slower than the typical rate. The normal heart rate range for adults is between 60 and 100 beats per minute.
Sinus rhythm is when your heart is beating regularly and normally. Sinus bradycardia means that your heart is beating regularly, but slower than normal. Sinus bradycardia is usually a benign arrhythmia (especially in very active people). That means while it's slower than expected, it also isn't harmful.
While bradycardia is a medical condition on its own, it often happens along with or because of other conditions. In those cases, bradycardia is often treated more like a symptom than a separate condition.
When you have bradycardia, your heart is beating slower than the average adult heart. This becomes a problem when your heart is pumping too slowly to keep up with your body’s demand for oxygen. That lack of blood flow and oxygen affects your entire body, especially your brain and heart.
Advertisement
For many people, bradycardia doesn’t cause any symptoms. This is especially true for people who are very physically active and have bradycardia because their hearts are more efficient. For people whose hearts can’t or don’t compensate, the symptoms tend to cause the following:
These symptoms happen because of how bradycardia affects your heart and your brain.
The average human brain weighs about 3 pounds — about 1.6% of the total weight of a 180-pound person. Despite its small size, the brain gets between 15% and 20% of the blood that comes out of your heart. If there isn’t enough blood flow, that affects your brain function.
Bradycardia symptoms often look a lot like the symptoms of heart failure. Bradycardia can also look like angina, which is chest pain or pressure that’s a warning sign of heart disease.
Bradycardia can happen for a wide range of reasons. Many of the other most common reasons include those listed below.
Other conditions include:
Bradycardia is not contagious (but some of the conditions that cause it are).
A doctor can diagnose bradycardia based on a combination of a physical exam and tests that measure your heart rate and analyze your heart rhythm.
The most likely tests for bradycardia include:
Lab tests are also possible for bradycardia, most of which can help rule out other problems. These tests include:
Other tests are possible if you have bradycardia, but many of these are only necessary if healthcare providers suspect you have another condition or problem. Your healthcare provider is the best person to explain the additional tests they recommend running and why.
If you have bradycardia but don’t have any symptoms, it’s unlikely that you need treatment. For those who do have symptoms, bradycardia is almost always treatable and is sometimes curable. If you have bradycardia because of another medical condition, sometimes treating that condition is all it takes to stop your bradycardia. An example of this is when you have bradycardia because of a medication you’re taking.
There are two primary ways to treat bradycardia.
If bradycardia is causing significant problems such as dangerously low blood pressure, an intravenous (IV) or injectable medication such as atropine can cause your heart to beat faster. Treatments like this are usually hospital-specific because people receiving these medications may need monitoring and additional care.
You can also take medications daily by mouth to help improve your heart function, including how strongly your heart beats or your heart rate.
This involves a device with electrical contacts that touch or attach to the skin of your chest. These contacts allow a mild electrical current to enter your body and cause your heart to beat. For people who need a permanent pacemaker or whose bradycardia will likely be short-lived, temporary cardiac pacing is an effective short-term treatment.
For many people with bradycardia, a permanent pacemaker is the best way to treat this condition. This is especially effective with conditions like sick sinus syndrome, where your heart’s natural pacemaker cells aren’t working properly.
While a permanent pacemaker can’t cure this condition entirely, it can be a long-term solution that treats this condition and keeps it from being a problem. Most pacemakers can last for several years, and some have batteries that can last more than a decade.
Receiving a permanent pacemaker usually involves surgery to implant the pacemaker device, which will deliver electrical pulses to your heart muscle. During this procedure, an electrophysiologist or surgeon will make a small pouch underneath your skin where your pacemaker will go. They’ll then place and connect wires (sometimes called leads) to various points on your heart.
For some people, surgery to implant a pacemaker is potentially avoidable. That’s because there are newer leadless pacemakers for bradyarrhythmias that are implantable using a catheter-based procedure. This procedure involves using a tube-like catheter device that a doctor inserts through an incision made into a major blood vessel. The provider can then steer the catheter up to and into your heart, where they can implant the pacemaker directly inside. These devices are very small (not much bigger than a large multivitamin pill), and you can go home much sooner than you would with surgery.
Complications from bradycardia are more likely to happen when this condition goes too long without treatment. That’s why a timely diagnosis and prompt treatment are so important.
The side effects or complications that are possible from medication vary widely based on what drugs you receive or the drugs you're already taking. Your healthcare provider is the best person to answer this question because they can tailor their answer to meet your specific situation, needs and circumstances.
Bradycardia is not a condition you should attempt to care for on your own without help from a healthcare provider. If you suspect you have it, you should see your provider (and sooner is better than later).
If you receive treatment for bradycardia, you should begin to feel better as that treatment happens. Many medications that treat this condition start to work quickly (especially IV medications). If you need a pacemaker, your symptoms should get better immediately after surgery, and you should feel better overall as you recover from the procedure.
Most people will recover from a pacemaker implantation procedure within a few weeks. However, your healthcare provider is the best person to tell you more about what you should expect and how long it will probably take for you to recover.
For many people, preventing bradycardia isn't possible. This is especially true when it comes to bradycardia which happens because you're in very good physical shape or bradycardia which happens naturally as you age.
Bradycardia is only preventable in cases where it happens because of the following:
In all other situations, bradycardia happens unpredictably. Because you can’t predict when it will happen, you can’t prevent it. However, many people will still develop bradycardia because of aging regardless of what they do to reduce their risk.
For many people, bradycardia doesn’t cause symptoms and isn’t a problem. This is especially true for people who have bradycardia because they’re in good physical shape.
For people who do have symptoms or problems because of bradycardia, you’re more likely to have a good outcome with early diagnosis and treatment. Delays in treatment, especially when bradycardia happens because of certain conditions, usually increase your risk of complications or death.
Bradycardia can be a life-long problem, or it can be short-lived. The underlying cause is usually what decides how long it will last. Bradycardia is more-likely to be a short-term problem when it happens because of drugs (prescription or recreational) or with other short-term conditions.
Overall, your healthcare provider is the best person to tell you whether or not this condition will be a short-term concern or if you'll have it for the rest of your life. In most cases where you have symptoms and you'll have it for the rest of your life, you'll need to take medication daily or have surgery to implant a pacemaker.
If you have bradycardia with symptoms, you should do the following:
You should see your healthcare provider at least once a year for an annual physical, regardless of whether or not you have bradycardia. This yearly visit is a key way for your healthcare provider to catch a wide range of healthcare problems early, especially ones that don’t have symptoms you can feel.
If you do have bradycardia but don’t have symptoms, you should see your provider if you notice any new symptoms or any changes in your overall health. If you do have symptoms, you should also see your provider if you notice your symptoms changing, especially in ways that are affecting your daily life and routine.
You should go to the hospital if you develop symptoms of bradycardia quickly or if you have symptoms that get worse or change suddenly.
You should also go to the hospital right away if you have any of the following symptoms (which can also be symptoms of much more serious problems like a heart attack):
A note from Cleveland Clinic
Bradycardia is a condition where you may not have symptoms or a problem, especially if it happens for certain reasons. Still, it’s normal to feel nervous or worried if you have unanswered questions now or the potential for future problems. Fortunately, bradycardia is a condition that’s almost always treatable. Your healthcare provider can also give you guidance and advice that will help prepare you for what you’re facing and what’s to come.
Last reviewed on 06/23/2022.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy