A heart attack (myocardial infarction) is a medical emergency where your heart muscle begins to die because it isn’t getting enough blood flow. A blockage in the arteries that supply blood to your heart usually causes this. If a healthcare provider doesn’t restore blood flow quickly, a heart attack can cause permanent heart damage and death.
A heart attack (myocardial infarction) is an extremely dangerous condition that happens because you don’t have enough blood flow to some of your heart muscle. This lack of blood flow can occur because of many different factors but is usually related to a blockage in one or more of your heart’s arteries.
Without blood flow, the affected heart muscle will begin to die. If you don’t get blood flow back quickly, a heart attack can cause permanent heart damage and/or death.
A heart attack is a life-threatening emergency. If you think you or someone you’re with is having a heart attack, call 911 (or your local emergency services phone number). Time is critical in treating a heart attack. A delay of even a few minutes can result in permanent heart damage or death.
When a heart attack happens, blood flow to a part of your heart stops or is far below normal, which causes injury or death to that part of your heart muscle. When a part of your heart can’t pump because it’s dying from lack of blood flow, it can disrupt the pumping function of your heart. This can reduce or stop blood flow to the rest of your body, which can be deadly if someone doesn’t correct it quickly.
Every year, more than 800,000 people in the U.S. have a heart attack. Most heart attacks are due to coronary artery disease, which is the most common cause of death in the United States.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Many people feel pain in their chest during a heart attack. It can feel like discomfort, squeezing or heaviness, or it can feel like crushing pain. It may start in your chest and spread (or radiate) to other areas like your left arm (or both arms), shoulder, neck, jaw, back or down toward your waist.
People often think they’re having indigestion or heartburn when they’re actually having a heart attack.
Some people only experience shortness of breath, nausea or sweating.
Heart attacks can have many symptoms, some of which are more common than others.
Heart attack symptoms that people describe most often include:
People assigned male at birth (AMAB) are likely to have different heart attack symptoms than people assigned female at birth (AFAB). People AFAB are less likely to have chest pain or discomfort that feels like indigestion. They’re more likely to have shortness of breath, fatigue and insomnia that started before the heart attack. They also have nausea and vomiting or pain in the back, shoulders, neck, arms or abdomen.
Advertisement
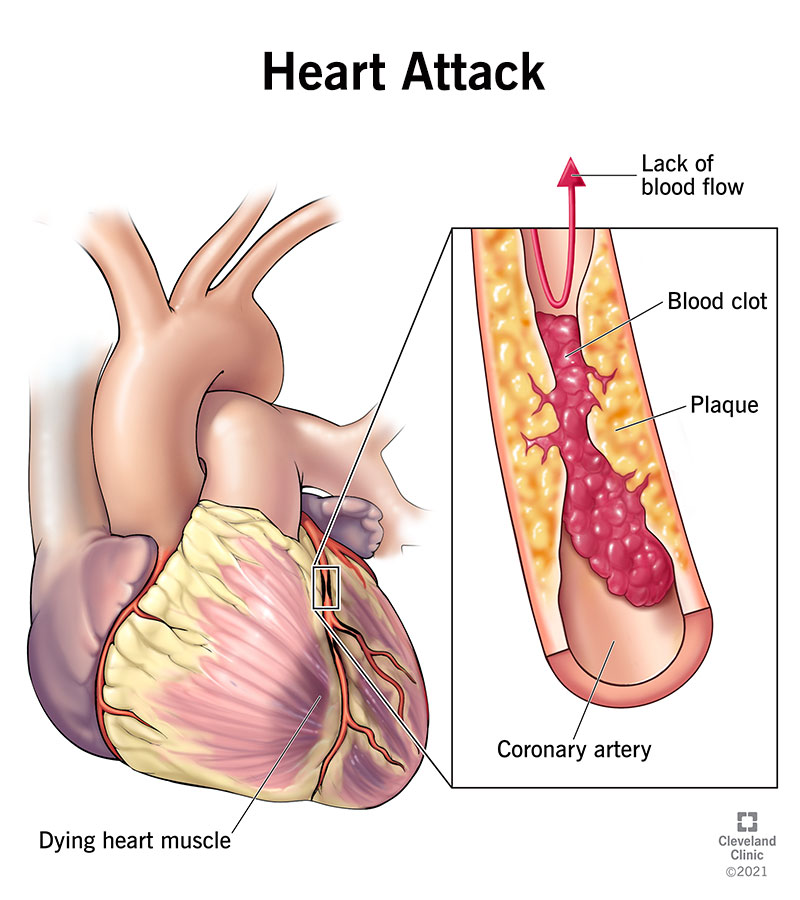
Most heart attacks happen because of a blockage in one of the blood vessels that supply your heart. Most often, this occurs because of plaque, a sticky substance that can build up on the insides of your arteries (similar to how pouring grease down your kitchen sink can clog your home plumbing). That buildup is called atherosclerosis. When there’s a large amount of this atherosclerotic buildup in the blood vessels to your heart, this is called coronary artery disease.
Sometimes, plaque deposits inside the coronary (heart) arteries can break open or rupture, and a blood clot can get stuck where the rupture happened. If the clot blocks the artery, this can deprive the heart muscle of blood and cause a heart attack.
Heart attacks are possible without ruptured plaque, but this is rare and only accounts for about 5% of all heart attacks. This kind of heart attack can occur for the following reasons:
Several key factors affect your risk of having a heart attack. Unfortunately, some of these heart attack risk factors aren’t things you can modify:
Complications associated with heart attacks include:
Advertisement
Healthcare providers usually diagnose heart attacks in an emergency room setting. If you have heart attack symptoms, you should undergo a physical examination. A provider will check your pulse, blood oxygen levels and blood pressure and listen to your heart and lung sounds. They’ll also ask you about the symptoms you experienced. They might ask someone who was with you to describe what happened.
A healthcare provider will diagnose a heart attack using the following:
Treating a heart attack means restoring blood flow to the affected heart muscle as soon as possible. This can happen in a variety of ways, ranging from medication to surgery. Treatment will likely include several of the following methods.
Supplementary oxygen
People having trouble breathing or with low blood oxygen levels often receive supplementary oxygen along with other heart attack treatments. You can breathe the oxygen either through a tube that sits just below your nose or a mask that fits over your nose and mouth. This increases the amount of oxygen circulating in your blood and reduces the strain on your heart.
Medications
These may include:
Percutaneous coronary intervention
Providers restore circulation to your affected heart muscle with a procedure called percutaneous coronary intervention (PCI) or angioplasty.
Opening your artery with a catheter is critical in restoring blood flow. The sooner that happens, the better the chance of a good outcome. Providers use a metric called “door-to-balloon time” to measure their ability to treat a heart attack. This is the average time it takes for people to undergo PCI after they first come into the emergency room. If you receive PCI, your provider may place a stent at the site of the blockage. The stent helps hold your artery open so another blockage doesn’t happen in the same spot.
Coronary artery bypass grafting
People who have severe blockages of their coronary arteries may undergo coronary artery bypass grafting (CABG). Providers often call this open-heart surgery or bypass surgery.
CABG involves using a blood vessel from elsewhere in your body (usually your chest, arm or leg) to construct a detour for blood. This reroutes blood around one or more blocked artery sections and brings blood to your heart muscle.
Treatment side effects vary by treatment and may include:
In general, your heart attack symptoms should decrease as you receive treatment. You’ll likely have some lingering weakness and fatigue during your hospital stay and for several days after. Your healthcare provider will give you guidance on rest, medications to take and more.
Recovery from the treatments also varies, depending on the method of treatment. The average hospital stay for a heart attack is between four and five days. In general, expect to stay in the hospital for the following length of time:
In general, there are many things that you can do that may prevent a heart attack. However, there are some factors you can’t change — especially your family history — that can still lead to a heart attack despite your best efforts. Still, reducing your risk can postpone when you have a heart attack and reduce the severity if you have one.
Although several risk factors can’t be modified, there are many ways you can help yourself and reduce your risk of a heart attack. These include:
Being an active contributor to your health doesn’t mean you have to make lifestyle changes all on your own. Ask your primary care provider and others on your healthcare team for help. They can provide the information and resources you need.
If you’ve already had a heart attack, your healthcare provider will recommend a cardiac rehabilitation program. This program’s goal is to reduce your chance of a second heart attack. These medically supervised programs provide counseling and focus on the same healthy living goals listed above.
The treatment you receive for a heart attack doesn’t end when you leave the hospital. Your risk of a second heart attack means you’ll need to take prescribed medicines and make changes to your daily life.
Recovery from a heart attack after leaving the hospital depends on the severity of the heart attack, how soon treatment began, which treatments you had and the health conditions you had — if any — before your heart attack.
Your healthcare provider can explain the next steps for your recovery and what you can expect. In general, most people can return to work or resume their usual activities anywhere between two weeks to three months after their heart attack. Cardiac rehab can help people gradually and safely increase their physical activity back to its prior level.
Today, many people survive a heart attack. But the outlook is worse for people who:
They may be at risk of another heart attack or of dying in the next six months or less. In these cases, providers will work to aggressively manage their risks.
Premenopausal people AFAB under age 45 have a better outcome than people AMAB of a similar age. Scientists believe this is because of estrogen’s heart-protective effects. But after menopause ends the protective benefits of estrogen, people AFAB fare worse than people AMAB. More specifically:
After a heart attack, you’ll continue to take medicines — some of which you received for immediate treatment of your heart attack — long-term. These include:
After you’ve had a heart attack, you’re at a higher risk of a similar occurrence. Your healthcare provider will likely recommend follow-up monitoring, testing and care to avoid future heart attacks. Some of these include:
If you have some of the heart attack symptoms above and think you’re having a heart attack, call your local emergency number. While they send help, ask if you should take an aspirin or other medicine. Don’t wait to call. Minutes matter when you’re having a heart attack.
Questions to ask your healthcare provider may include:
If you have any symptoms of a heart attack, it’s best to call 911 for multiple reasons:
A note from Cleveland Clinic
A blocked artery needs immediate care to prevent permanent heart damage. You may think that if your symptoms aren’t intense and severe, you’re not having a heart attack. But symptoms can be mild and it’s best to have a provider check them. Calling 911, rather than driving yourself or having someone else drive you, can be even more life-saving than you think. Time saved is a heart muscle saved, and that means a better chance of a good outcome for you.
Last reviewed on 02/15/2024.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy