Atrial fibrillation (Afib) is an irregular heart rhythm that begins in your heart’s upper chambers (atria). Symptoms include fatigue, heart palpitations, trouble breathing and dizziness. Afib is one of the most common arrhythmias. Risk factors include high blood pressure, coronary artery disease and having obesity. Untreated Afib can lead to a stroke.
Atrial fibrillation (also called Afib or AF) is an irregular heart rhythm (arrhythmia) that begins in the upper (atria) of your heart. If you have atrial fibrillation, the normal cycle of electrical impulses in your heart is interrupted. This leads to a fast, chaotic heart rhythm and poor movement of blood from your atria to your lower chambers (ventricles).
There are three main types of atrial fibrillation.
Afib, if untreated, can lead to a stroke and other serious medical complications. That’s why it’s important to learn the symptoms and talk with your healthcare provider about your personal risk factors.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Some researchers have called Afib the “new cardiovascular disease epidemic of the 21st century.” Afib is especially common among older adults. Over 33 million people age 55+ have been diagnosed globally. Estimates predict that 12 million people in the U.S. will have Afib by 2030. Afib causes nearly half a million yearly hospitalizations in the U.S. and leads to more and more deaths with each passing year.
While Afib can affect anyone, it’s more common among people of European descent. However, Black people who have Afib are more likely to have serious complications such as stroke or heart failure. People assigned female at birth (AFAB) are more commonly diagnosed than people assigned male at birth (AMAB).
Advertisement
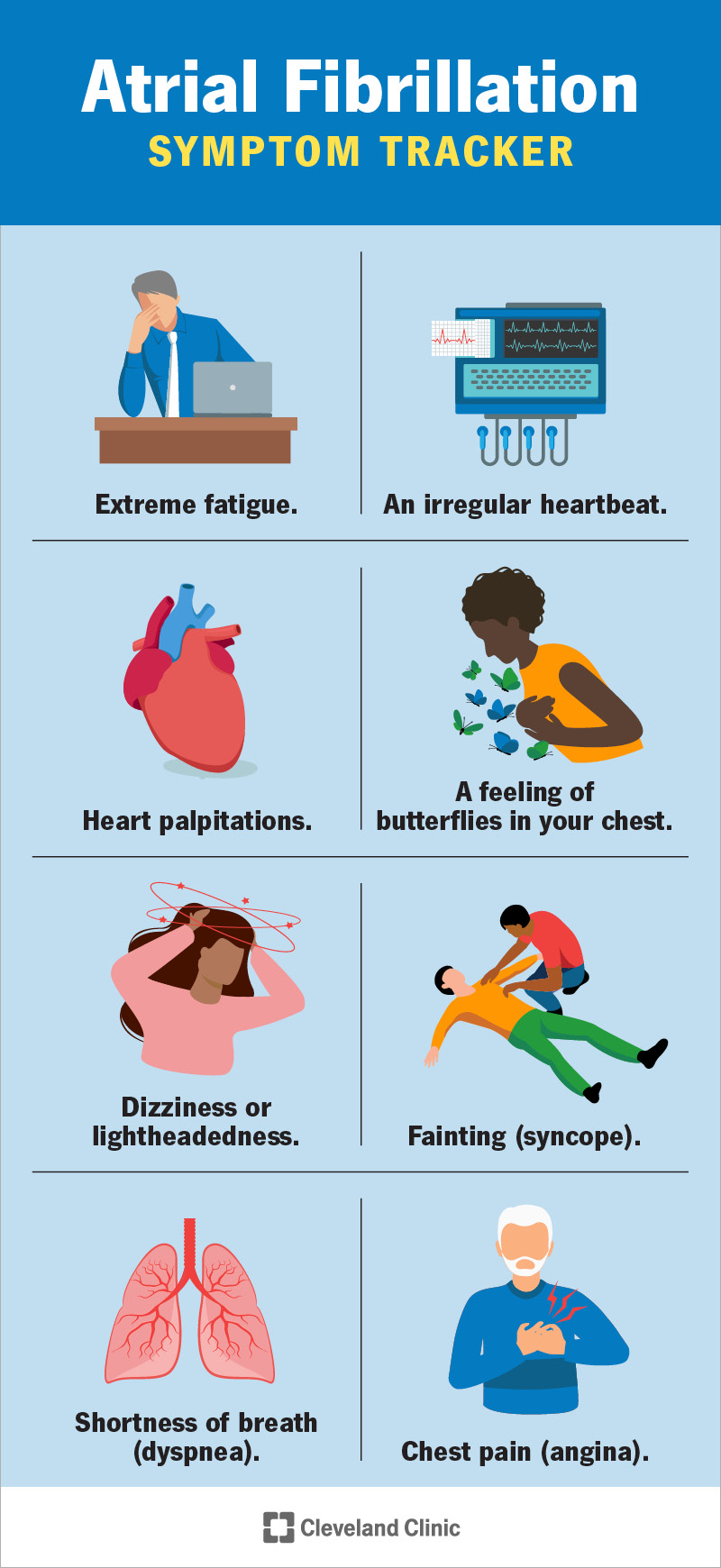
You might be wondering what Afib feels like. Some people with Afib have no symptoms. It depends on how fast your ventricles are beating. If they’re beating at a normal or slightly elevated pace, you probably won’t feel anything. But if your ventricles beat faster then you’ll start to notice symptoms. These can include:
If you have symptoms, keep a list of when they happen and share this information with your healthcare provider right away.
Atrial fibrillation can cause serious medical complications. So, it’s essential to learn the warning signs and to share them with your family and friends. In many cases, we need someone else to call 911 for us. Immediately call 911 (or your local emergency services) if you have the following symptoms or if you notice them in someone around you:
These are signs of bleeding in your brain, digestive system, or urinary tract. Many people with Afib need to take blood-thinning medications to lower the risk of Afib-related stroke. This medication is essential. But taking too high a dose can cause bleeding in your body.
People assigned female at birth may also have:
These are signs you may be having a stroke. Learn how to recognize these symptoms in yourself or others so you can act quickly. Every minute counts.
These symptoms can happen within an hour before having a cardiac arrest. In some cases, these symptoms might not appear at all, and a person could simply faint. If you or a loved one have Afib, it’s a good idea to talk with your healthcare provider about how to get help in medical emergencies. For those who live alone or spend lots of time alone, there may be no one home to call for help. Medical alert devices may be a life-saving resource.
Advertisement
If you think you have Afib symptoms, it’s important to call your healthcare provider right away to discuss how you’re feeling. Your provider may ask you to check your pulse. If it feels erratic or weak, that could be a sign you’re in Afib.However, sometimes you might not notice any changes in your pulse, especially if your Afib isn’t advanced. You may instead just feel tired or out of breath. You may not know if your symptoms are from Afib or something else. That’s why a call to your provider is essential.
When you’re in Afib, your heart’s electrical system isn’t working as it should. Your electrical impulses are chaotic, leading to an irregular and rapid heartbeat. When you feel your pulse isn’t right, you might wonder what’s going on inside your heart. It’s helpful to learn more about the differences between a normal heartbeat and what happens when you’re in Afib.
Your heart pumps blood to the rest of your body. During each heartbeat, your two atria contract, followed by your two lower chambers (ventricles). These actions, when timed perfectly, allow your heart to work as an efficient pump. Your heart’s electrical system controls the timing of your heart’s contractions. And your sinoatrial (SA) node is normally in charge of that electrical system. This node is located in your right atrium. When your SA node fires an impulse, electrical activity spreads through your right and left atria (“atrium” is singular and “atria” is plural). Both atria then contract and force blood into your ventricles.
The impulse then travels to the atrioventricular (AV) node, located near the middle of your heart. From there, the impulse moves to your ventricles, causing them to contract and pump blood out of your heart to your lungs and the rest of your body. This process repeats with every heartbeat. The SA node directs the timing of the electrical impulses and keeps your heart pumping smoothly.
You can think of your SA node as the conductor of an orchestra. Your SA node is responsible for keeping your heart beating at the proper pace and rhythm. Likewise, an orchestra conductor directs all the musicians to keep the music flowing at the right tempo, sometimes faster and sometimes slower.
Normally, your SA node adjusts to your level of activity. For example, it increases the rate of impulses when you exercise and decreases the rate when you sleep. With the SA node conducting your heart’s rhythm, you are in “normal sinus rhythm.” This means your heart is beating at a regular rhythm and pace, about 60 to 100 times per minute.
If you have atrial fibrillation, your SA node isn’t directing your heart’s electrical rhythm. Instead, many different impulses rapidly fire at the same time, causing a fast, chaotic rhythm in your atria. As a result, your atria can’t contract or pump blood effectively into your ventricles. Your ventricles contract irregularly, causing a rapid irregular heartbeat.
It’s as if in the middle of a concert, two more conductors walked onto the stage and started waving their batons. The musicians would no longer know who to follow or what to do. The music would lose its rhythm and harmony.
Fortunately, there are many ways to bring back your heart’s rhythm and harmony if you have Afib. It all starts with a visit to your healthcare provider, who can run some tests and make a diagnosis.
Changes or damage to your heart’s tissue and electrical system cause atrial fibrillation. Usually, coronary artery disease or high blood pressure causes those changes. Often a trigger heartbeat causes atrial fibrillation to begin. But sometimes it’s hard to know the cause of that triggered heartbeat. For some people, there is no identifiable cause. Research is constantly providing new information to help us learn more about the
Afib often runs in families. So, if a close family member has Afib, you have a “family history” and therefore a higher chance of developing it, too.
We don’t fully know the connections between atrial fibrillation and anxiety. Research has identified Afib as a cause of anxiety (if you have Afib, you might worry about your symptoms or quality of life). But few studies have explored anxiety as a cause of Afib. We do know that anxiety can raise your risk of cardiovascular disease and causes a 48% higher risk of cardiac death. However, we need more research to find out if anxiety disorders can cause Afib.
To diagnose atrial fibrillation, your healthcare provider will first ask you some questions. You’ll share information about your diet and physical activity, family history, any symptoms you’ve noticed and risk factors. It’s OK if you don’t know all the answers but share as much as you can. Your experiences and knowledge are essential tools to help your provider make a diagnosis. Your provider will then give you a physical exam that includes:
This exam will help your provider understand your baseline health and how your body is functioning.
In addition to the physical exam, your provider may run some tests to make an atrial fibrillation diagnosis. These tests include:
In some cases, your provider may want to check how your heart works in your daily life. If so, you’ll be asked to wear a Holter monitor (for one or two days) or a portable event monitor (for up to one month) to record your heart’s activity.
An EKG records your heart’s electrical impulses and can show if you have atrial fibrillation.
The main goals of Afib treatment include:
Based on your symptoms, your healthcare provider will likely first prescribe medications to see if they help.
Medications to treat Afib may include:
Any medications can cause side effects. Rate control and rhythm control medications may make your arrhythmia worse or impact your lungs, liver or other organs. Blood thinners can cause bleeding, indigestion or a heart attack. Usually, the benefits of taking these medications outweigh your risk of side effects. It’s important to discuss all risks and side effects with your provider.
If medications don’t help your Afib, you may need a procedure or surgery.
Many procedures can be non-invasive, and newer treatment methods and technologies are constantly developing. Talk with your provider about the options that are best for you.
If you have paroxysmal Afib, your symptoms may go away on their own without treatment. However, paroxysmal Afib can progress to persistent Afib depending on your risk factors. And both persistent Afib and long-standing persistent Afib require treatment to avoid serious complications. As Afib progresses, it becomes more serious and harder to treat. Afib can’t be cured, but its symptoms can be managed. Talk with your healthcare provider about the management and treatment plan that’s best for you.
The older we get, the greater our risk for atrial fibrillation. When we hit 65, our risk especially increases. Besides increasing age, high blood pressure is a huge risk factor. High blood pressure causes 1 in 5 cases of Afib. You also have a higher risk of developing Afib if you have any of the following conditions:
In addition, certain lifestyle factors like smoking, alcohol consumption and recreational drug use can raise your risk.
While exercise strengthens your heart, some athletes who exercise intensely for long periods of time could have a higher risk of Afib. In such cases, reducing the exercise intensity usually helps.
An estimated 1 in 3 people with Afib don’t know they have it. That’s why it’s important to know the risk factors and talk with your healthcare provider. If you’re at risk, you should have your heart and pulse checked regularly so you can catch problems early.
If you have other medical conditions or a family history of Afib, you may feel like it’s impossible to prevent. It’s true that some risk factors can’t be changed. However, the four major risk factors for Afib that we can change are obesity, physical inactivity, excessive alcohol consumption and tobacco use. Here are some tips to lower your risk:
As you lower these risk factors, you will also see other benefits like reduced blood pressure, lower cholesterol levels and weight loss. When it comes to heart health, each positive lifestyle change has a ripple effect. The more changes you can make, the more benefits you will enjoy in the long run.
There’s no single schedule to follow. It all depends on your symptoms and treatment plan, and whether you need follow-ups after a procedure. So, it’s important to talk with your provider and make a plan together. Make sure you go to all your scheduled appointments. Keep track of the medications you’re taking, and bring a list of your medications to every appointment. It’s also a good idea to keep the list in your wallet so it’s with you in emergencies.
At each visit, be sure to share any new symptoms or problems you’re having, such as side effects from medication.
Your provider will ask you questions, but it’s important to ask your own questions, too. For example, ask for advice on how to reduce your risk factors. Starting a new diet or exercise plan can feel overwhelming. Your provider will offer advice and also connect you with others who can help, such as dietitians. You may also want to ask about available health and fitness programs, including those that support your mind-body connection.
Finally, be sure to ask your provider before taking over-the-counter medicines, such as those for cold and flu, and nutritional supplements. Sometimes these products can affect your heart rate or interact with your prescription medications.
A note from Cleveland Clinic
Atrial fibrillation is a complex heart condition that can seem scary, confusing or overwhelming. But whether you suspect you might have Afib, were recently diagnosed or have been living with it for years, you’re not alone. You’re one of the millions of people who are learning new strategies for managing Afib while still enjoying life. That’s why it’s important to talk with your healthcare provider and learn more about available resources and support communities.
It’s also helpful to learn about the benefits and risks of treatment options. All medications or procedures carry some risks. But when it comes to Afib, treatment is essential for supporting your heart and reducing your chances of having a stroke. Your provider will work with you to choose the best approach. With treatment, monitoring and lifestyle changes, you can live a long and healthy life with Afib.
Last reviewed on 05/01/2022.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy