Testicular cancer is the most common cancer affecting people assigned male at birth aged 15 to 35. The most common sign to look out for is a painless lump in your testicle. Testicular cancer that’s diagnosed and treated early has an excellent cure rate.
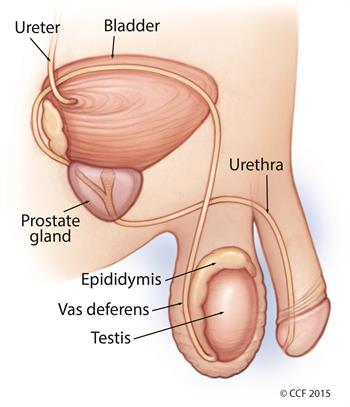
Testicular cancer forms when malignant (cancer) cells develop in the tissues of one or (less commonly) both testicles. Your testicles are two walnut-shaped sex glands that produce sperm and the hormone testosterone. They sit inside a sac of skin that lies below your penis called the scrotum.
Like any cancer, testicle cancer is a serious condition. Fortunately, testicular cancer is highly treatable and curable.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
About 90% of all testicular cancer arises from germ cells in your testicles that clump together to form a mass or tumor. Germ cells eventually develop into sperm. Two types of testicular cancer arise from germ cells.
Some testicular cancer tumors consist of both seminoma and non-seminoma cells.
Testicular cancer is rare, affecting only about 1 in 250 people with testicles in their lifetimes. Still, it’s the most common cancer among people assigned male at birth aged 15 to 35.
Advertisement
The most common sign of testicular cancer is a painless lump in your testicle. Other symptoms include:
These symptoms can occur with other conditions, too, so don’t panic if you notice them. Still, schedule a visit with your provider to be sure. Delays in diagnosis allow cancer cells time to spread, making the disease harder to treat.
Testicular cancer develops when cells multiply faster than usual, eventually forming a lump or tumor. Researchers aren’t sure what causes cells to behave this way. They do know that the cells that become testicular cancer are usually germ cells.
Advertisement
Several factors may increase your testicular cancer risk. Risk factors don’t cause testicular cancer, but they may increase its likelihood of developing.
Risk factors for testicular cancer include:
Your provider may diagnose testicular cancer after investigating a lump or other change in your testicle you found during a self-exam. Sometimes testicular cancer gets diagnosed during a routine physical exam.
Common procedures and tests to help diagnose testicular cancer include:
Other tests may include:
Diagnosis also involves cancer staging. Staging provides important information that will guide treatment decisions, such as tumor size and whether the cancer’s spread.
Treatment depends on several factors, including your health, treatment preferences, cancer stage, and tumor type. Seminomas tend to grow more slowly and respond better to radiation therapy than non-seminomas. Both kinds of testicular cancer tumors respond well to chemotherapy treatments.
If testicular cancer involves both seminoma and non-seminoma tumors, your provider will treat it as a non-seminoma.
Surgery to remove the cancerous testicle is the most common treatment for testicular cancer, regardless of cancer stage or tumor type. In some cases, your provider may also remove your lymph nodes.
Your provider may also perform surgery to remove tumors that have spread to your lungs or liver.
Radiation therapy uses high-dose X-rays to kill cancer cells. Radiation might be used after surgery to prevent the tumor from returning. Usually, radiation is limited to the treatment of seminomas.
Chemotherapy uses drugs such as cisplatin, bleomycin, and etoposide to kill cancer cells. Chemotherapy has improved the survival rate for people with both seminomas and non-seminomas. Depending on your cancer, you may receive chemotherapy instead of surgery. It may be used before an RPLND procedure or after a radical inguinal orchiectomy. Chemotherapy may also be used to treat cancer that’s returned (recurred) following remission.
Testicular cancer isn’t preventable, but you can perform testicular self-exams (TSE) to identify changes in your testicles that you should bring to your provider’s attention. Your provider should know about lumps, nodules, hardness or a testicle that’s become bigger or smaller.
Many providers recommend performing a testicular self-exam monthly.
You can complete a TSE in as little as two minutes. Many providers recommend performing a testicular self-exam monthly.
To do a self-exam, follow these steps.



If you notice a change in the size of your testicles or feel a lump, contact your healthcare provider.
You should also get a physical exam yearly.
The prognosis for testicular cancer is excellent. This form of cancer is treated successfully in more than 95% of cases. Even people with unfavorable risk factors have, on average, a 50% chance of being cured.
Testicular cancer is curable. While a cancer diagnosis is always serious, the good news about testicular cancer is that it is treated successfully in 95% of cases. If treated early, the cure rate rises to 98%.
Testicular cancer can be fatal, but this is rare. Still, early detection makes a big difference in your prognosis. The earlier you see your provider and receive a diagnosis, the greater your chances of being cancer-free.
Many people wonder how having a testicle removed will impact their sex drive and fertility. One testicle is usually all you need to make enough testosterone to keep your hormone levels healthy and maintain your sex drive. You should still be able to get an erection and ejaculate.
In some instances, people with lymph nodes removed can get an erection but may have difficulty ejaculating.
Talk to your provider about any risks related to treatment. If you’re concerned about your fertility, sperm banking, or freezing your sperm for later, use may be an option.
A note from Cleveland Clinic
Don’t delay scheduling a provider visit if you notice a change in one or both testicles. Most people would rather avoid or postpone exams that involve close inspection of their genitals. When it comes to cancer, though, timing is essential. Depending on your cancer type, early treatment can cure testicular cancer.
Last reviewed on 05/02/2022.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy