A breast MRI is an imaging test that produces very clear pictures of breast tissue. Healthcare providers mainly use it to evaluate known breast cancer. But they also use it in addition to mammography and ultrasound to screen for and diagnose breast cancer and other abnormalities.
Breast MRI (magnetic resonance imaging) is a type of imaging study that uses a large magnet, radio waves and a computer to produce detailed images of breast tissue. Unlike mammograms, a breast MRI doesn’t use X-rays (radiation).
Some of the most common reasons to perform a breast MRI include:
Depending on the reason for a breast MRI, it may or may not require injection of contrast dye (called gadolinium). For many breast MRIs, a technologist or nurse will place an IV in your arm so they can inject contrast dye during the test. This helps a radiologist see normal and abnormal structures in your breast more clearly. This dye is different from the one used during CT scans.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Healthcare providers use mammograms and breast MRIs (and ultrasounds) to help detect breast cancer and other abnormalities.
However, mammograms are usually the first option for screening and diagnosis of breast cancer, particularly as mammograms are the only imaging test able to reliably identify microcalcifications — an early presenting sign of some breast cancers.
There are also differences in how the two imaging tests work.
| Mammogram | Breast MRI |
|---|---|
| Uses X-rays. | Doesn’t use X-rays. |
| Compresses (squeezes) your breasts. | Doesn’t compress your breasts. |
| Doesn’t use contrast dye (no IV necessary). | Usually requires contrast dye (an IV is necessary). |
| Images acquired over two to three minutes. | Images acquired over 17 to 20 minutes. |
| Mammogram | |
| Uses X-rays. | |
| Breast MRI | |
| Doesn’t use X-rays. | |
| Compresses (squeezes) your breasts. | |
| Breast MRI | |
| Doesn’t compress your breasts. | |
| Doesn’t use contrast dye (no IV necessary). | |
| Breast MRI | |
| Usually requires contrast dye (an IV is necessary). | |
| Images acquired over two to three minutes. | |
| Breast MRI | |
| Images acquired over 17 to 20 minutes. |
Your healthcare provider may recommend a breast MRI for several reasons, including:
Providers often recommend this test to provide more detail after diagnosing breast cancer. It can:
Breast MRIs may also be a helpful test to further evaluate lumpectomy sites in the years following breast cancer treatment. This is because scarring and recurrent breast cancer can look the same on mammography and ultrasound.
An MRI can find some small breast tumors that a mammogram might miss, but it can also produce false-positive and false-negative results. For example, sometimes, a benign (noncancerous) piece of tissue in your breast can show up as a bright spot on the image, much like breast cancer. This would be a false-positive result. In any case, if a radiologist sees something in your breast tissue that doesn’t look normal, they may order additional tests such as a breast ultrasound or a biopsy to determine exactly what the finding is.
Alternatively, not all cancers will always show up on MRI that radiologists may be able to better see on other imaging tests, like a mammogram. This would be a false-negative result. This is one reason why the American Cancer Society and the U.S. Preventative Services Task Force don’t recommend breast MRI as a screening test by itself.
Advertisement
A radiologist or radiology technologist performs a breast MRI.
A radiology technologist is a medical professional who’s specially trained and certified to perform MRI scans, but they don’t interpret the results or give medical opinions or advice.
A radiologist is a medical doctor who performs and interprets imaging tests to make a diagnosis. They offer medical advice based on the findings.
Before your breast MRI, it’s important to tell your provider if you:
The magnetic resonance imaging (MRI) scanner uses a strong magnet and radio wave signals that can cause heating or possible movement of some metal objects in your body. This could result in health and safety issues. It could also cause some implanted electronic medical devices to malfunction.
If you have metal-containing objects or implanted medical devices in your body, your healthcare team needs to know about them before your exam. Please tell your provider and MRI technologist if you have any of the following:
You won’t be able to wear the following devices during your MRI:
Talk to the provider you see for these devices (such as your endocrinologist) to learn how you should go about the MRI.
Advertisement
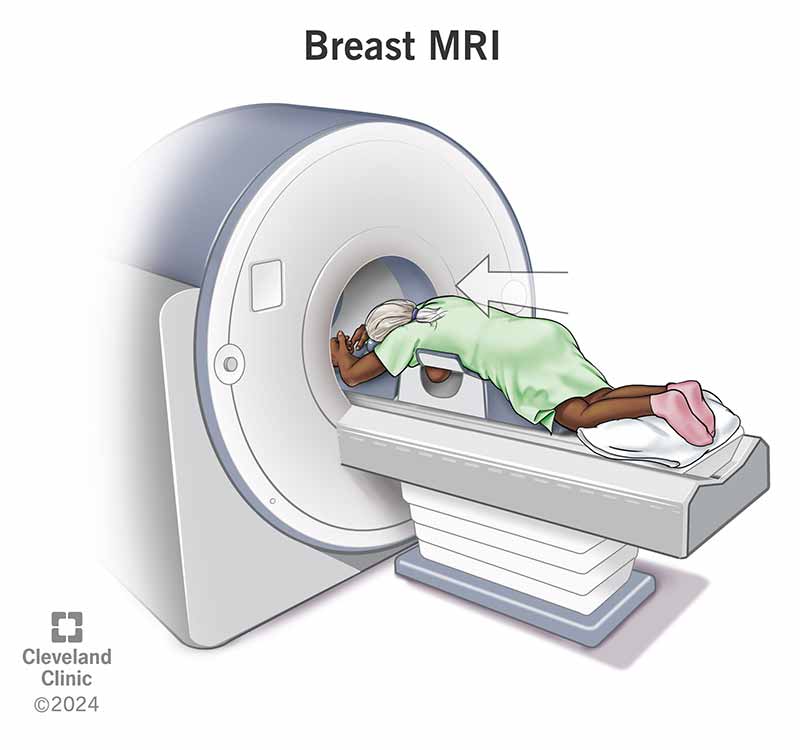
During a breast MRI, you can expect the following:
Many people are nervous about an MRI scan because they’re afraid of being enclosed in a tight space. It’s true that the older machines were narrow with very little head-to-ceiling space. But newer machines are larger and have significantly improved in terms of comfort. For example, newer MRI machines are open at both ends. They also have wider openings, shorter total lengths, more head-to-ceiling space and are fully ventilated (a fan will blow a gentle stream of air on you).
If you’re worried you may be too anxious during the procedure, talk to your provider. You may be able to take a sedative before the procedure so you’re more relaxed.
Generally, you can resume your usual activities after a breast MRI.
However, if your exam was an MRI breast biopsy, follow the at-home instructions your provider gives you. If you took a sedative for your exam, you’ll need someone else to drive you home.
Although many facilities plan for 40 to 60 minutes for a breast MRI, the scan itself only lasts up to 20 minutes. The extra time is used for screening questionnaires, IV placement and proper positioning for the exam.
There’s very little risk to getting a breast MRI as long as you and your technologist follow the safety guidelines.
There’s a chance you might have an allergic reaction to the contrast dye (gadolinium), but this is very rare. Reactions are usually mild, and your healthcare team will quickly treat it if it happens.
It’s important to tell your provider and technologist if you’re pregnant or breastfeeding (chestfeeding).
Depending on whether you got a breast MRI for screening purposes, diagnostic purposes or to evaluate known cancer, your MRI report may look different. In any case, your provider who ordered the breast MRI will discuss your results with you.
Radiologists all use the same standardized system to describe screening and diagnostic breast imaging (including mammogram, ultrasound and MRI) results. This system is called the Breast Imaging Reporting and Data System (BI-RADS). This system categorizes results on a scale of 0 through 6.
| BI-RADS category | Definition | Explanation |
|---|---|---|
| 0 | Incomplete. | This result means the radiologist may have seen a possible abnormal area, but they need further images to evaluate it, such as a diagnostic mammogram or an ultrasound. This result may also mean that the radiologist wants to compare your most recent breast MRI with older ones to see if there’ve been changes in the area over time. |
| 1 | Negative. | This result means the radiologist didn’t find a significant abnormality on the images. |
| 2 | Benign (noncancerous) finding. | This result means that the radiologist found a benign (noncancerous) area in your breast, such as benign cysts, lymph nodes or fibroadenomas. The radiologist records this finding to help when comparing it to future breast imaging tests. |
| 3 | Probably benign finding. | The findings in this category have a greater than 98% chance of being benign (noncancerous). But as it’s not proven to be benign, the radiologist wants to monitor it to be sure it doesn’t change over time. You’ll likely need additional imaging (such as MRI) in six months. |
| 4 | Suspicious abnormality. | This result means a finding(s) is not normal and has suspicious features suggesting it could be cancer. The radiologist will recommend a breast biopsy to get more information. The findings in this category can have a 2% to 95% chance of being a cancer. |
| 5 | Highly suggestive of malignancy. | The term “malignancy” refers to the presence of cancerous cells. This result means the findings look like cancer and have at least a 95% chance of being cancer. The radiologist will strongly recommend a breast biopsy of these findings. |
| 6 | Known biopsy-proven malignancy. | Radiologists use this result for findings on a mammogram or MRI that’ve previously been biopsied and are a known cancer. Healthcare providers use MRIs in this way to see the extent of the cancer and/or how well it’s responding to treatment. |
| BI-RADS category | ||
| 0 | ||
| Definition | ||
| Incomplete. | ||
| Explanation | ||
| This result means the radiologist may have seen a possible abnormal area, but they need further images to evaluate it, such as a diagnostic mammogram or an ultrasound. This result may also mean that the radiologist wants to compare your most recent breast MRI with older ones to see if there’ve been changes in the area over time. | ||
| 1 | ||
| Definition | ||
| Negative. | ||
| Explanation | ||
| This result means the radiologist didn’t find a significant abnormality on the images. | ||
| 2 | ||
| Definition | ||
| Benign (noncancerous) finding. | ||
| Explanation | ||
| This result means that the radiologist found a benign (noncancerous) area in your breast, such as benign cysts, lymph nodes or fibroadenomas. The radiologist records this finding to help when comparing it to future breast imaging tests. | ||
| 3 | ||
| Definition | ||
| Probably benign finding. | ||
| Explanation | ||
| The findings in this category have a greater than 98% chance of being benign (noncancerous). But as it’s not proven to be benign, the radiologist wants to monitor it to be sure it doesn’t change over time. You’ll likely need additional imaging (such as MRI) in six months. | ||
| 4 | ||
| Definition | ||
| Suspicious abnormality. | ||
| Explanation | ||
| This result means a finding(s) is not normal and has suspicious features suggesting it could be cancer. The radiologist will recommend a breast biopsy to get more information. The findings in this category can have a 2% to 95% chance of being a cancer. | ||
| 5 | ||
| Definition | ||
| Highly suggestive of malignancy. | ||
| Explanation | ||
| The term “malignancy” refers to the presence of cancerous cells. This result means the findings look like cancer and have at least a 95% chance of being cancer. The radiologist will strongly recommend a breast biopsy of these findings. | ||
| 6 | ||
| Definition | ||
| Known biopsy-proven malignancy. | ||
| Explanation | ||
| Radiologists use this result for findings on a mammogram or MRI that’ve previously been biopsied and are a known cancer. Healthcare providers use MRIs in this way to see the extent of the cancer and/or how well it’s responding to treatment. |
The results of your MRI will be available in your electronic medical records account (if you have one) and should be available to the provider who ordered the test within one to two business days of your exam. Your provider will discuss the results with you.
A note from Cleveland Clinic
A breast MRI is a helpful tool for screening, diagnosing and evaluating breast cancer and other abnormalities. If you need a breast MRI and are worried about the procedure or have questions about it, don’t be afraid to ask your healthcare provider. They’re available to help and support you.
Last reviewed on 12/13/2022.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy