Mammograms are an essential breast cancer screening and diagnostic tool. Using low-dose X-rays, they can show abnormal (usually noncancerous, or benign) areas or tissues in your breast and can help detect cancer before you have symptoms.
A mammogram is a low-dose X-ray of breast tissue. Healthcare providers use mammograms, or mammography, to look for early signs of breast cancer before symptoms develop. This is called a screening mammogram. Providers also use mammography to look for any abnormalities if you develop a new symptom, such as a lump, pain, nipple discharge or breast skin changes. This is called a diagnostic mammogram.
Aside from skin cancer, breast cancer is the most common cancer that affects people assigned female at birth and represents 14% of all new cancer diagnoses in the United States. While breast cancer treatment therapies continue to improve and have contributed to a reduction in cancer-related deaths, early diagnosis through screening mammograms has a greater overall impact on survival rates.
Most findings in mammograms are benign, or noncancerous. In fact, fewer than 1 in 10 people who need additional tests after a mammogram have cancer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In general, there are two main types of mammograms:
In the United States, digital mammography has replaced conventional (film) mammography, also known as analog mammography. Digital and conventional mammography both use X-rays to produce an image of your breast. The difference is that the image is stored directly on film in conventional mammography, whereas digital mammography provides an electronic image that’s stored as a computer file. Digital mammography allows healthcare providers to save the file electronically and to more easily evaluate and share the images.
A digital mammogram usually involves at least two pictures of each breast taken at different angles — typically from top to bottom and from side to side — and provides a two-dimensional (2D) view.
3D mammography, also known as digital breast tomosynthesis (DBT), is a newer type of mammogram in which each breast is compressed once and a machine takes several low-dose X-rays as it moves in an arc over your breast. A computer then puts the images together, which allows healthcare providers to see your breast tissues more clearly in three dimensions.
Many studies have revealed that 3D mammography increases cancer detection, including lower-grade cancers, and decreases false-positive rates. Given these advantages, 3D mammography for both screening and diagnostic mammograms is rapidly becoming the go-to option for mammograms.
A screening mammogram is a routine (usually annual) mammogram that healthcare providers recommend to look for signs of cancer or abnormal breast tissue before you have symptoms. Screening mammography helps with the early detection of breast cancer. Early detection allows for early treatment, which may be more effective than if the cancer is found at a later stage.
A routine screening mammogram usually includes at least two pictures of each breast taken at different angles, typically from top to bottom and from side to side. If you have breast implants, you’ll need additional images.
Healthcare providers order a diagnostic mammogram if a screening mammogram shows abnormal tissue or there’s a new breast issue.
While both types of mammograms use the same machines, diagnostic mammography uses additional imaging techniques, such as spot compression, supplementary angles or magnification views and is supervised by the radiologist at the time of the study.
Advertisement
Mammograms can help detect cancer, but they can’t diagnose cancer.
While mammograms can show abnormal breast tissue, they can’t prove that an abnormal area in your breast is cancer. Rather, mammograms are an essential tool for helping healthcare providers decide whether you need additional testing, such as a breast biopsy. A breast biopsy can determine if tissue is cancerous or noncancerous.
Several organizations, including the American Cancer Society and the American College of Radiology, recommend yearly screening mammograms beginning at age 40 for all people assigned female at birth (AFAB) with an average risk of developing breast cancer. People AFAB at average risk are those with less than a 15% lifetime risk of developing breast cancer. Your personal risk of a new breast cancer increases as you age.
People AFAB with an increased risk of developing breast cancer may need to have screening mammograms at a younger age since they may develop breast cancer at an earlier age. Your provider may recommend supplemental screening with other tests, such as a breast MRI, based on breast cancer risk assessment.
Occasionally, people assigned male at birth (AMAB) may also have a high-risk level because of their family history and may also have screening mammography. In general, though, about 1 out of 100 people AMAB develop breast cancer.
If you have any of the following risk factors, talk to your provider about when you should start getting annual screening mammograms:
Advertisement
Mammography is 85% to 90% accurate. Mammograms have improved the ability to detect breast abnormalities before they are large enough to be felt. However, it’s possible that a mass you can feel might not show on a mammogram. Any abnormality that you feel when examining your breasts should be evaluated by your healthcare provider. They may recommend a diagnostic mammogram.
A healthcare provider called a radiology technologist or a mammographer performs a mammogram. They have specialized training in performing a mammogram safely and properly. A board-certified radiologist who is specially qualified to interpret mammograms then views and interprets the mammogram images. They send the results to your healthcare provider who will then share them with you.
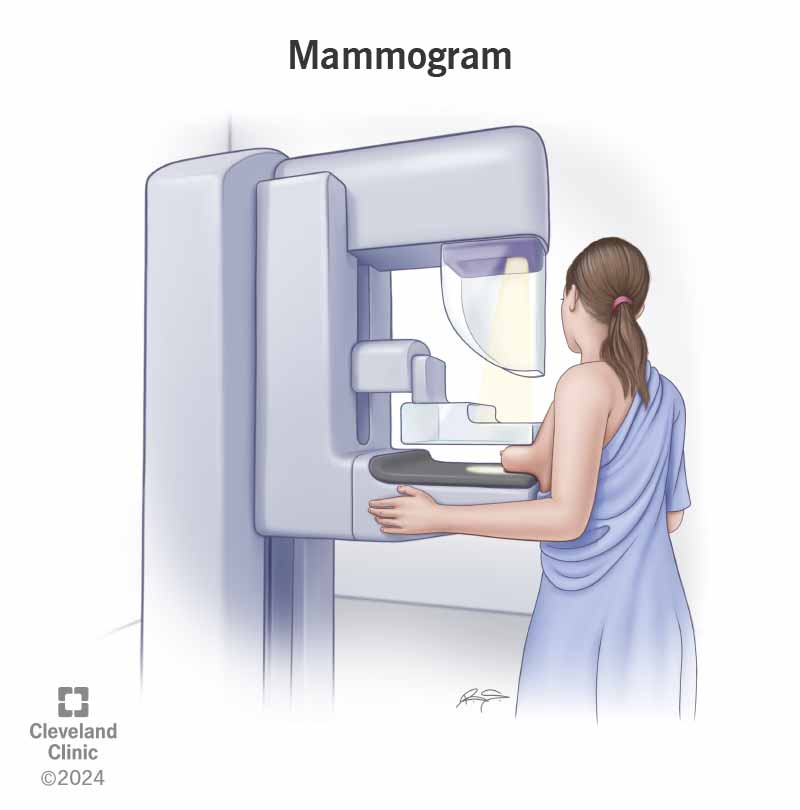
A mammogram uses an X-ray machine that’s designed to only look at breast tissue. The machine takes X-rays at lower doses than X-rays used to look at your bones.
During a mammogram, you place your breast on a support plate attached to the X-ray machine. A technologist then squeezes your breast with a parallel plate called a paddle. The machine produces X-rays that pass through your breast to a detector located on the opposite side. The detector transmits electronic signals to a computer to form a digital image. These images are called mammograms.
Breast compression is necessary for a mammogram to hold your breast still and minimize movement, which can cause the X-rays to look blurry. Compression also evens out the shape of your breast so that the X-rays can travel through a shorter path to reach the detector. This allows for a lower radiation dose and improves the quality of the image.
There are a few things to do or keep in mind when scheduling your mammogram, including:
On the day of your mammogram, follow these guidelines:
A mammogram involves the following steps:
Undergoing a mammogram feels uncomfortable for some people due to the pressure on your breast tissue from the compression. For some people, it’s painful. The good news is that a mammogram is a brief procedure and the discomfort doesn’t last long. If you feel intense pain, tell the technologist immediately.
The level of discomfort you may feel depends on a few factors, including:
Most people will be able to resume their normal activities immediately after their mammograms.
Screening mammograms usually take about 15 to 20 minutes. Diagnostic mammograms may take longer due to the extra images that are needed.
Mammograms expose your breasts to small amounts of radiation, but the benefits of mammography outweigh any possible harm from the radiation exposure.
If there’s any chance you might be pregnant, let your healthcare provider and technologist know. Although mammograms are generally safe during pregnancy, healthcare providers usually recommend postponing screening mammograms if you don’t have an increased risk of developing breast cancer.
You’ll likely get your mammogram results within a few days, although this can vary. A radiologist looks at your mammogram and then sends the results to you and your healthcare provider.
Contact your provider or the facility where you got your mammogram if you don’t receive your results within a month.
You’ll receive a result letter that gives basic information about the result and should be easy to understand. The letter may inform you of normal results or the need to return for additional imaging. Your mammogram report will also include information about your breast density, which is how much fibrous and glandular tissue you have in your breasts as compared to fatty tissue. The denser your breasts, the more difficult it can be to see abnormal areas on mammograms. Having dense breasts also raises your risk of getting breast cancer. This information is now mandated by law to be provided in your report. If you have any questions about your results, don’t be afraid to ask your healthcare provider.
Radiologists and healthcare providers use a standard system in medical reporting to describe screening and diagnostic mammogram findings called the Breast Imaging Reporting and Data System (BI-RADS). This system sorts the results into categories numbered 0 through 6.
Incomplete (BI-RADS 0)
This result means the radiologist may have seen a possible abnormal area, but they need specialized images to evaluate it, like a diagnostic mammogram or an ultrasound. It may also mean that the radiologist wants to compare your most recent mammogram with older ones to see if there have been changes in the area over time.
Negative (BI-RADS 1)
This result means the radiologist didn’t find a significant abnormality to report. Your breast(s) don’t have any masses, distorted structures or suspicious calcifications. In this case, negative means there are no abnormal areas or findings.
Benign (noncancerous) finding (BI-RADS 2)
This result means that the radiologist found a benign (noncancerous) structure in your breast, such as benign calcifications, cysts, lymph nodes or fibroadenomas. The radiologist records this finding to help when comparing it to future mammograms.
Probably benign finding (BI-RADS 3)
This result is only given after a diagnostic mammogram. The findings in this category have a > 98% chance of being benign (noncancerous). But since it’s not proven to be benign, the radiologist wants to monitor it to be sure it doesn’t change over time. You’ll likely need another mammogram in six months.
Suspicious abnormality (BI-RADS 4)
This result is only given after a diagnostic mammogram. It means the finding(s) could be cancer but the radiologist recommends a breast biopsy for more information. The findings in this category can have a wide range of suspicion levels, and it’s sometimes divided into further categories, including:
Highly suggestive of malignancy (BI-RADS 5)
This result is only given after a diagnostic mammogram. The term "malignancy" refers to the presence of cancerous cells. This result means the findings look like cancer and have at least a 95% chance of being cancer. The radiologist strongly recommends a breast biopsy.
Known biopsy-proven malignancy (BI-RADS 6)
Radiologists only use this result for findings on a mammogram that have previously been diagnosed as cancer by a biopsy. Healthcare providers use mammograms in this way to see how well the cancer is responding to treatment.
A radiologist will carefully examine your screening mammogram to look for masses, asymmetries and calcifications, especially if they’re new from prior studies. Based on the result of the screening mammogram, you may be called back for a diagnostic study.
If you have a normal mammogram it means that the radiologist didn’t find any issues or abnormal areas in your breasts in the images. If you have a normal mammogram, it’s important to continue to get mammograms according to recommended time intervals. Screening mammograms are most helpful when a radiologist can compare them to ones you’ve had in the past to look for changes in your breasts.
If a mammogram shows one or more suspicious regions, the radiologist will likely recommend additional mammogram views, other imaging tests such as a breast ultrasound, or a breast biopsy.
Your healthcare provider will go over the next steps with you if you receive an abnormal mammogram report.
Having silicone or saline breast implants and resulting scar tissue makes it more difficult for radiologists to see all of your breast tissue and possible issues on regular mammograms.
To help the radiologist see as much breast tissue as possible, people with implants usually have two extra pictures done on each breast in addition to the four standard pictures taken during a screening mammogram. These extra images are called implant displacement (ID) views.
For ID views, the technologist gently pushes your breast implant back against your chest wall, pulls your breast forward over it and then compresses your breast. This allows for better imaging of the front part of each breast.
It’s important to let the mammogram facility know you have breast implants when scheduling your mammogram and to let your technologist know on the day of your mammogram.
No, but let your technologist know when you had your last vaccine dose and in which arm.
People who have received a COVID-19 vaccine can have swelling in the lymph nodes in their armpits in the arm that they got the shot. While swelling in your lymph nodes is a normal sign that your immune system is building protection against COVID-19, it’s possible that this swelling could cause temporary lymph node enlargement visible on a mammogram.
A note from Cleveland Clinic
Mammograms are an essential breast cancer screening tool. They can also help monitor benign breast conditions over time. While the procedure can be uncomfortable and waiting for results can be anxiety-inducing, it’s important to get your mammogram at the recommended age and time intervals based on your risk of developing breast cancer. If you have any questions about your risk of getting breast cancer or the mammogram process, talk to your healthcare provider. They’re there to help you.
Last reviewed on 04/05/2022.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy