Your sternum, or breastbone, is a flat, vertical bone at the center of your chest that protects your organs and muscles. It connects to other bones and muscles and forms part of your ribcage, which protects your heart and lungs. Many different conditions can cause sternum pain, but most aren’t serious. See your provider if you have any concerns.
Your sternum is a flat, T-shaped bone at the center and front of your chest. Your sternum protects the organs and muscles inside your chest from injury. It also connects to other bones and muscles with cartilage. It forms part of your ribcage, which protects your heart and lungs. Another name for your sternum bone is your breastbone.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your sternum (breastbone) works with your ribcage to protect the organs within your chest. This includes your:
Your breastbone also provides support — it connects to other parts of your skeletal system, including your clavicle (collarbone) and first six sets of ribs. Other muscles in your chest and upper belly (abdomen) connect to your sternum, as well.
Your sternum doesn’t help with movement in your chest or torso. But cartilage that connects your sternum to your ribs helps with minor motions that occur every time you take a breath.
The breastbone location is at the center and front of your chest. You can find it in your upper chest in front of your thymus. It connects to your clavicles, which run horizontally (from side to side) above it.
Your thymus gland is located behind your sternum (breastbone). This gland is part of your lymphatic system. It’s in charge of training special white blood cells called T-lymphocytes (T-cells).
Advertisement
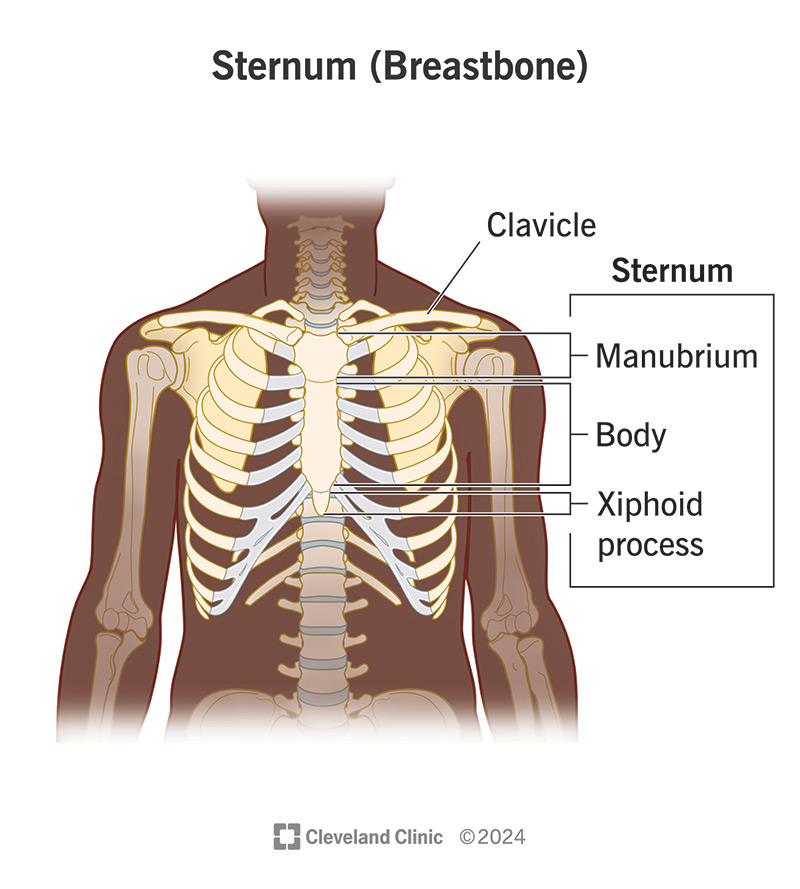
Your sternum anatomy consists of three bony parts. These parts include:
The tip of the sternum is called the xiphoid process. It’s thinner and narrower than the rest of the sternum. Its shape can vary, but it usually forms into a small point at the bottom of the sternum.
Your sternum measures about 6 inches long from top to bottom. You could compare the shape of your sternum to an upside-down sword. This is because the wide part at the top resembles a handle. The body of the sternum is long and flat, like the blade of a sword. And the xiphoid process at the end of the sternum looks like the tip of a sword.
Advertisement
Many issues with your sternum and its surrounding bones and muscles can cause sternum pain. In addition, you may experience substernal pain — discomfort that occurs below or behind your sternum. This type of pain is usually due to gastrointestinal conditions. Some common causes of sternum or substernal pain include:
Costochondritis is a condition that causes inflammation in the cartilage that attaches your ribs to your sternum. An infection, injury or arthritis can cause the condition. Costochondritis causes sharp, stabbing rib pain and tenderness. You usually feel it in your sternal area and the first three sets of ribs, but it can spread to your arms and shoulders. You may also notice warmth and tenderness in the area.
Pectus carinatum is a condition that causes your sternum to stick out more than it should. Other names for the condition include pigeon chest and keel chest because of how it makes your chest appear. Most people with pectus carinatum don’t have symptoms. But, you may experience chest pain when in specific positions or participating in certain activities.
A sternal fracture occurs when you break your sternum bone, most often due to blunt force trauma. Sternum fractures commonly occur due to auto accidents. They also happen because of sports injuries and falls. There are two types of sternum fractures:
Your sternoclavicular joint is the area in your body where your clavicle connects to your sternum. Although rare, you can sometimes develop problems in this joint area due to infections, injuries or arthritis. You’ll experience pain and discomfort if you have an injury there.
Your collarbone (clavicle) connects to the top corners of your sternum. Since the two are closely connected, if you injure your collarbone, you’ll feel pain and discomfort in your sternum, as well. You can injure your collarbone through accidents, sports injuries and falls.
A muscle strain, or a pulled muscle, can occur when you injure a tendon or muscle. Many tendons and muscles are connected to your sternum. Therefore, injuries to a muscle or tendon can also affect your sternum. Muscle strains occur due to overuse, playing sports and coughing too hard.
A hiatal hernia happens when the top of your stomach moves past your diaphragm and into your chest. This affects the area behind your chest and can cause substernal pain (the area behind your sternum). Hiatal hernias are the most common type of hernia.
Acid reflux occurs when stomach acid causes irritation and inflammation that wears away the lining of your esophagus. This can cause substernal pain. The condition most often affects people with gastroesophageal reflux disease (GERD).
Pleurisy is a condition that causes inflammation in your pleurae — the sheets of tissue between your ribcage and lungs. Some autoimmune diseases, lung conditions, and bacterial or viral infections can cause pleurisy. This can also cause substernal pain.
Bronchitis is a condition that causes inflammation in the primary airways leading to your lungs — your trachea (windpipe) and bronchi — causing substernal pain. This inflammation causes your lungs to fill with mucus, leaving you with a nagging cough that can last for weeks.
Pneumonia is a condition that causes inflammation in the air sacs (alveoli) in your lungs. After the alveoli inflame, they fill with fluid, which can cause sharp chest pains. You may feel this pain behind your sternum.
The symptoms and signs of sternum pain will vary depending on the cause. The most common symptom you may experience is pain and discomfort in the center area of your chest. Other symptoms you may experience include:
You may not experience any symptoms, or you may have some chest pain while performing certain activities and being in certain positions.
These symptoms often worsen when lying down.
These symptoms often worsen with eating.
Treatment of sternum pain will vary depending on the cause.
The most common treatment option for costochondritis is rest. You need to give your chest and ribcage time to heal. Your healthcare provider may also recommend over-the-counter (OTC) pain medications like nonsteroidal anti-inflammatory drugs (NSAIDs). Rarely, your provider will inject you with a corticosteroid to reduce the inflammation.
The most common treatment options for pectus carinatum are bracing and surgery. With bracing, you wear a brace around your chest 24 hours a day for a long time (months to years). This provides pressure from the back and the front to move your sternum back to its usual position.
Surgery for pectus carinatum involves a procedure called the Ravitch procedure. A surgeon will make a cut (incision) into your chest to remove the cartilage in the front of your chest. Then, they’ll make a small cut in the front of your breastbone, press it into its usual position and anchor it in place.
Treatment for a sternal fracture depends on the type and severity of your injury. You may only need rest and pain medication for mild cases. In more severe cases, you may require surgery to put your sternum back into its proper position.
Treatment for a sternoclavicular joint injury also depends on the severity of your condition. For mild cases, your healthcare provider may recommend rest, avoiding activities that trigger pain and pain relievers. More severe cases may require surgery.
Treatment for a collarbone (clavicle) injury depends on the severity. For mild cases, your healthcare provider may recommend putting your arm in a sling to keep it from moving, or a collar bone fracture brace. They may also recommend icing it to reduce swelling and pain relievers to help with the pain. You may need to see a physical therapist to help improve your arm motion and strengthen your shoulder. In severe cases, you may require surgery.
You can treat most muscle strains using OTC pain relievers, ice and heat, massage and rest. Sometimes, prescription muscle relaxants can be prescribed.
More severe injuries may require surgery.
If a hiatal hernia doesn’t cause any symptoms, you don’t necessarily need treatment. But if you have symptoms, they won’t get better without treatment. You can manage mild cases of hiatal hernias with acid reflux medication or lifestyle changes such as small meals, avoiding lying down after eating and weight loss. You may need surgical care for more severe cases.
You may be able to treat acid reflux with lifestyle changes, including eating well-balanced meals, avoiding certain trigger foods, quitting smoking and reducing your alcohol and caffeine intake. If you have chronic acid reflux or GERD, you may need medication to reduce the amount of acid in your stomach. You can get some medications over the counter (like antacids). Other medications, like proton pump inhibitors (PPIs), may require a prescription.
Treatment for pleurisy depends on the cause. Your healthcare provider may recommend pain relievers for symptom relief. You may need a medication to treat an infection. In severe cases, you may need a procedure called a thoracentesis, where your provider removes fluid from your lungs.
Treating this depends upon the cause. Certain viruses like flu or COVID can be treated with antiviral medication. In some cases, if you’re having trouble breathing, your provider may prescribe a drug that helps open your airways (bronchodilator) or corticosteroids for the inflammation.
Treatment for pneumonia depends on whether a bacterial, viral or fungal infection caused your condition. If a bacterial infection caused your condition, your healthcare provider may prescribe an antibiotic. They may prescribe an antiviral if you have a viral infection, and they may recommend an antifungal if you have a fungal infection.
You should visit your healthcare provider if:
Your provider can help diagnose the cause of your pain and develop a treatment plan.
If you’re experiencing chest pain, you may worry that you’re having a heart attack. But heart attack pain differs from sternum pain. Most of the time, sternum pain begins suddenly. If you’re having a heart attack, you’ll likely experience other, specific signs before it starts. Symptoms of a heart attack may include:
If you’re experiencing any of these signs, seek immediate medical attention.
A note from Cleveland Clinic
Your sternum (breastbone) is a vertical bone at the top of your chest that protects your organs and supports your muscles and other bones. Several different health conditions can cause sternum pain or substernal pain, but most aren’t serious. If you have persistent sternum pain, reach out to your healthcare provider to find out the cause and receive treatment. While sternum pain is different from the pain you’d experience during a heart attack, make sure to know the signs of when to get emergency medical attention.
Last reviewed on 02/27/2024.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy