A penrose drain is a straight, flexible tube that drains fluid from a surgery site. It channels blood, lymph and other fluids that can collect in a wound outside your body. This prevents infection and can help you heal. It’s important to care for your drain properly to prevent infection.
A penrose drain is a soft, flexible rubber tube that drains fluid away from a wound. After surgery, blood, lymphatic fluid (lymph) and other fluids can collect at the surgery site or wound. These fluids can become infected if bacteria aren’t drained. A penrose drain directs the fluid collecting inside the wound outside your body. It can reduce the risk of infection and help you heal faster.
You may also hear your healthcare provider call it a “straight” or “open” drain. Imagine a soft straw. A penrose drain is so soft it compresses against your wound right away. It keeps your wound open (preventing skin from closing over it), allowing fluid to drain.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
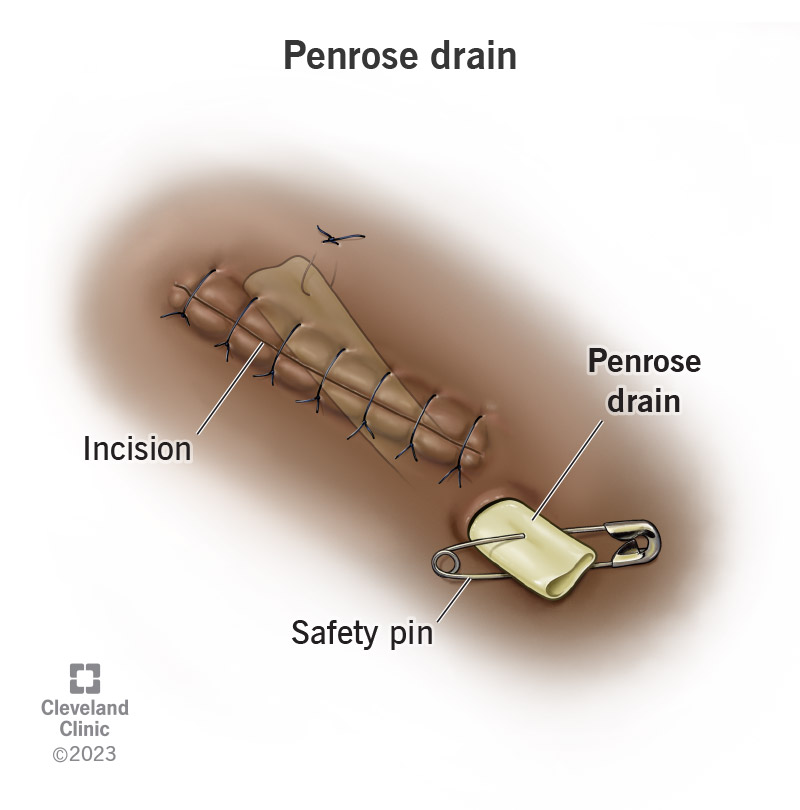
It’s a type of passive drain, which means its design relies on gravity — not a suction feature — to draw fluid out of your wound. Your surgeon will place most of the drain inside the cut and leave a small part sticking out. Usually, they suture (stitch) the drain so it doesn’t slide out. Sometimes, they’ll attach a safety pin to the end of the drain to ensure it stays outside your body.
Gravity naturally pulls the fluid outside your body. The drain just provides the route.
A penrose drain can keep you from getting an infection after surgery. It can also drain infected fluid away from your wound. Infection is one of the most common avoidable complications after surgery.
Your surgeon may place a penrose drain to:
Advertisement
Penrose drain care involves changing the dressing. The dressing includes a piece of gauze on your skin that collects the fluid that seeps from the drain and a piece of gauze that covers the drain.
Your surgeon may ask you to log information about the drainage, including how much fluid the gauze absorbs and what it’s like (its color and smell). These notes provide important information about how you’re healing.
Plan to change your dressing near a sink because you’ll need to wash your hands to keep bacteria out of the wound. It’s a good idea to gather all the materials you’ll need beforehand, including:
Here’s what you do:
Throw away the gloves, old dressing and tape. Wash your hands again.
Most people need to change it at least twice a day, but follow your provider’s instructions. You’ll need to change the dressing if it comes loose or gets too wet. Keeping your skin dry reduces your risk of infection.
It’s a good idea to change it at the same time each day and log when you do it so you can share this information with your provider.
It depends on your procedure, how big the wound is and how much drainage there is. Often, fluids drain for a few days following surgery.
Follow your provider’s instructions on when you need to return to have your drain removed.
Call your healthcare provider if your drain slips or comes loose. They may need to secure it. Contact your provider immediately if you notice signs of an infection, including:
Contact your provider if you have questions about caring for your drain or whether your wound is healing properly.
Advertisement
A Jackson-Pratt drain also drains fluid away from a wound. Unlike a penrose drain, a Jackson-Pratt drain is an active drain. It has a squeezable bulb that hangs outside your body. Squeezing the bulb creates pressure that pulls the fluid from your wound. Often, the bulb has markings that let you know exactly how much fluid has drained.
Instead of describing drainage based on how wet the gauze is (as with a penrose), a Jackson-Pratt drain shows how many cubic centimeters (CCs), milliliters (mLs ) or ounces (oz) of fluid you’ve lost.
A note from Cleveland Clinic
Follow your healthcare provider’s instructions while caring for your drain and wound. Many details, including how often you should change the dressing and when you should return to have the drain removed, depend on your surgery and healing progress. In the meantime, note how much fluid you’re losing and how the wound looks. Share this information with your provider to help them monitor your recovery.
Last reviewed on 09/19/2023.
Learn more about the Health Library and our editorial process.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy